Robert M. Bernstein, MD and Michael B. Wolfeld, MD
Dermatologic Surgery 2016; 42(6): 710-14
The use of robotic technology to harvest grafts in a follicular unit extraction hair transplant procedure (FUE) has been available since 2011. A new capability of the robotic system is to select follicular units based on the number of hairs they contain in order to increase the hair/wound yield when harvesting grafts. This bilateral controlled study of 24 patients was designed to evaluate this functionality. Results showed that, compared to random follicular unit harvesting (the method performed by current robotic systems), robotic follicular unit graft selection produced more hairs per harvest attempt (2.60 vs. 2.22) and more hairs per graft (2.72 vs. 2.44). The clinical benefit of follicular unit graft selection (as measured by the increase in hairs per harvest attempt) was 17.0%. The clinical benefit (as measured by the increase in hairs per graft) was 11.4%. Results were statistically significant at p<.01.
Introduction
After years of relatively slow adoption since its introduction into the medical literature in 2002, ((Rassman WR, Bernstein RM, McClellan R, Jones R, et al. Follicular Unit Extraction: Minimally invasive surgery for hair transplantation. Dermatol Surg 2002; 28(8): 720-7.)) Follicular Unit Extraction (FUE) is experiencing unprecedented growth. In 2006, FUE represented only 7.4% of all hair transplant procedures performed world-wide with a growth rate of a mere 0.4% over the two-year period 2004-2005. By 2014, 48.5% of all hair transplant procedures were performed using FUE, with a bi-annual growth rate of 16.3%. This represents a 40-fold increase in growth over the earlier period. ((Hair Restoration Practice Census, published by the International Society of Hair Restoration Surgery (ISHRS) in 2015.))
The first robotic FUE procedures were performed using the ARTAS® System in late 2011, with only a handful of cases that year. ((Bernstein RM. Integrating Robotic FUE into a hair transplant practice. Hair Transplant Forum Intl. 2012; 22(6): 228-229.)) By 2014, 12.6% of all hair transplants and 26% of all FUE cases were performed using automated devices.[2] With the use of robotic devices increasing so rapidly (3 systems operating in 2011 and over 120 worldwide in 2015), ((Data supplied by Restoration Robotics, Inc.)) the interest in robotic technology has expanded from researchers and a few physician-early adopters to all those involved in surgical hair restoration.
Over the five-year period since its introduction, robotic technology has advanced dramatically, with new systems being far more nuanced and user friendly and having transection levels that continue to improve. ((Avram MR, Watkins SA. Robotic Follicular Unit Extraction in Hair Transplantation. Dermatol Surg 2014; 40(12): 1319-27.)) A significant limitation of the robotic system, however, has been its inability to select follicular units while harvesting – something that is done intuitively when follicular unit extraction is performed by the human hand.
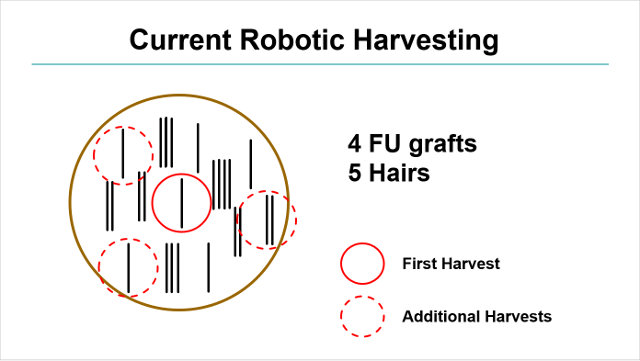
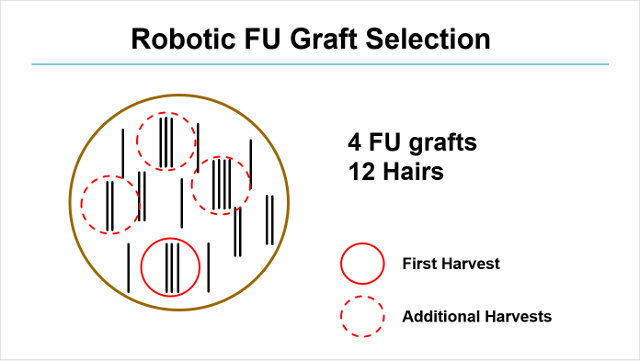
When Follicular Unit Extraction (FUE) is accomplished manually, the doctor visually chooses larger follicular units in order to maximize the amount of hair harvested through the smallest number of recipient wounds. The current iteration of the robotic system used for FUE (ARTAS®) randomly selects follicular units irrespective of their hair content.[5], ((Rose PT, Nussbaum B. Robotic Hair Restoration. Dermatologic Clinics. Advances in Cosmetic Dermatology. 2014; 32(1): 97-107.)) A new capability of the robot is to select follicular units based on the number of hairs they contain in order to increase the hair/wound yield when harvesting follicular unit grafts. This paper examines the new technology for robotic follicular unit extraction (R-FUE) and presents data from a bilateral controlled study, designed to evaluate its benefits.
Follicular Unit Graft Selection
In robotic follicular unit graft selection, the discriminatory features of the robotic optical system are used to identify the hair content of each follicular unit and then an algorithm is used to automatically select the desired larger follicular units for harvesting. The technology has the ability to preferentially select follicular units of 2 or more hairs (enable mode). The present study examines the effects of skipping only 1-hair follicular units as these have the lowest hair-to-wound ratio, they are the easiest for the robot to select optically, and skipping 1-hair FUs does not significantly decrease the total yield (number of hairs).
In Follicular Unit Transplantation via strip harvesting (FUT) the entire harvested tissue is used; therefore, the number of hairs/graft will be approximately the same as the ratio of hairs per follicular unit that occurs naturally on a person’s scalp (i.e., on average about 2.2-2.4 hairs/FU). Most hair transplant procedures are designed with this in mind.
In FUE, the benefit of follicular unit graft selection is to obtain the maximum amount of donor hair through the smallest number of donor wounds. When performed efficiently by robotic follicular unit graft selection, the resultant number of hairs per graft produced can often exceed what is needed for a specific hair restoration procedure. For example, at 2.7 hairs/graft, the follicular units are too large for all of them to be transplanted intact. In this case, there may be too many four-hair units for a natural distribution and too few ones for the hairline.
In these cases, the doctor can: 1) program the robot to be less specific, 2) make a “second pass” to harvest additional 1-hair grafts, or 3) use stereo-microscopic dissection to divide the largest follicular units into smaller ones. In all three scenarios, the hair-to-wound ratio (most hair per recipient wound) can still be superior to randomly selected follicular units.
The robot can be programmed to skip as many 1s as possible, even at the expense of significantly limiting the number of grafts per field (high setting), or skip only some 1s in order not to substantially reduce the total number of grafts harvested (low setting). The low setting also operates at a slightly faster speed than the more discriminatory high setting. The current study uses the algorithm that skips as many 1s as possible (high setting). At present, the discriminatory ability of the robot is imperfect and some 1-hair grafts still appear, even in the high setting.
Another variation of follicular unit graft selection is a “two-pass” technique (two-pass enable mode). In the first pass, the doctor harvests all FUs that contain more than 1-hair (using either the high or low setting described above) and in the second pass, the robot automatically goes back and harvests any 1s skipped in the first pass. This may be important in situations where the physician desires to harvest the maximum amount of grafts in a given area or to maximize the total grafts for the procedure. Another indication would be for patients with a large number of 1-hair grafts, such as Asians, for whom skipping all 1s would yield too few grafts.
Although initially it may be counterintuitive, the two pass-technique yields higher hair content than if follicular units were randomly selected. The reason is that selecting a 1-hair graft on the first pass can block the robot from harvesting a larger follicular unit in close proximity since a minimum distance (generally 1.7mm) is required between harvests (see Figures 1, 2). The current study looks at both the first and second passes of a two-pass technique and compares it to random follicular unit graft harvesting (disable setting).
Method
The current study was performed on twenty four, first-time hair transplant patients undergoing robotic follicular unit extraction for androgenetic alopecia. The ARTAS® robotic system (version 7.x) was used for graft harvesting. A 19-gauge dual-punch system was used which consisted of a 0.9mm (ID) sharp punch and a 1.1mm (ID) dull, punch rotating at 3,000 RPMs. The donor sites were spaced a minimum of 1.7mm apart.
The study used a bilateral controlled, randomized design. On the experimental side, follicular units were harvested using a high selection setting and a two-pass technique (enable mode). On the control side, follicular units were selected randomly (disable mode). A 3cm x 3cm skin tensioner with fiducial markings was used to stabilize the skin and allow the robotic device to create four non-overlapping harvested areas (of approx. 2cm x 2.5cm) on each side. (See Figure 3.) After the doctor examined the results of the study and control areas, the remainder of the harvesting was completed using the algorithm that best suited the needs of the patient.
The measurements include: the number of harvest attempts (HA), the number of grafts, and the number of individual hairs. Hair and graft counts were made using a Meiji stereo-microscope at 10x resolution. The calculated values were hairs/HA and hairs/graft.
The study measured the percent change (increase) in hairs/HA after one-pass of the two-pass algorithm compared to the random (disabled) mode and the percent change (increase) in hairs/HA after the two-pass technique compared to the random (disabled) mode. The same calculations were performed for hairs/graft. Any percentage increase of either the one-pass or two-pass techniques over the random mode, with respect to hairs/HA and hairs/graft, was considered to represent the “clinical benefit” of follicular unit graft selection.

Figure 3. Donor area showing experimental design
Results
Results showed that, compared to random follicular unit harvesting (disable mode), robotic follicular unit graft selection produced more hairs per harvest attempt (one-pass 2.60 and total for two-pass 2.50 vs. random 2.22) and more hairs per graft (one-pass 2.72 and total for two-pass 2.60 vs. random 2.44). Results were statistically significant at p<.01 using an unpaired two sample t-test (Figures 4, 5).
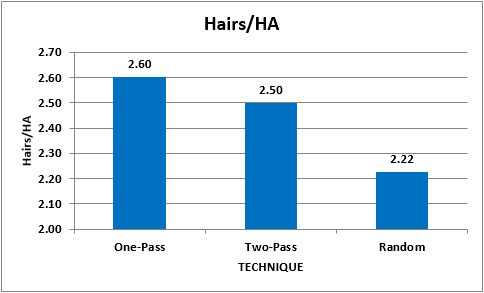
Figure 4. Average hairs per harvest attempt, n=24, unpaired t-test, p<.01
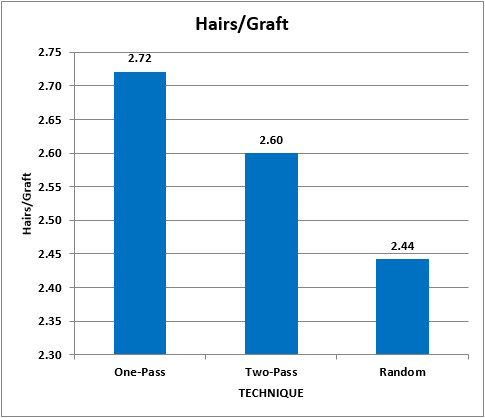
Figure 5. Average hairs per graft. n=24 patients, unpaired t-test, p<.01
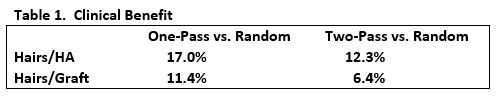
The clinical benefit of follicular unit graft selection (as measured by the increase in hairs per harvest attempt) after one-pass compared to the random mode was 17.0%. The clinical benefit of the two-pass technique compared to random harvesting (disable mode) was 12.3%. The clinical benefit (as measured by the increase in hairs per graft) after one-pass compared to the random mode was 11.4%. The clinical benefit of the two-pass technique compared to random harvesting (disable mode) was 6.4%. Results were statistically significant at p<.01 using an unpaired two sample t-test. (Table 1.)
Discussion
Follicular unit graft selection allows the clinician the ability to select larger follicular units during the harvest phase of an FUE procedure in order to maximize hair content and minimize wounding. Until now, this technique could only be performed by hand. The new functionality of the robotic system allows the automation of this important aspect of FUE and provides more versatility to the robotically-performed hair restoration procedure.
The successful application of robotic follicular unit graft selection is predicated on the team’s skill in stereo-microscopic dissection. Ironically, this is a skill that is best developed from years of dissecting donor strips (i.e. expertise in FUT). In all cases of FUE, it is incumbent upon physicians to train their staff in stereo-microscopic dissection in order to trim, count, and sort the follicular unit grafts accurately. When the technique of FUE graft selection is used to minimize donor wounds, the same skills are required to divide the grafts a-traumatically into smaller units or single hairs. Of course, this is a challenge for doctors that perform any of the FUE techniques (manual, motorized, or robotic) to the exclusion of FUT and, therefore, these authors recommend that a physician and his team be skilled in both types of procedures.
In the current study, the initial pass of the two-pass technique (in a high setting) yielded a hairs/graft content of 2.72. This is significantly greater than the approximately 2.2-2.4 hairs/graft generally needed for a hair transplant. If one dissected the follicular unit grafts of 4-hairs or greater, into 2- and 3- hair grafts, the hair/graft count can be reduced to the normal 2.24 hairs/graft. In this example, the total number of grafts would be increased by 21%, without increasing the number of donor wounds.
The higher number of hairs per graft (that exceeds the natural average) necessitates that a portion of the larger grafts are dissected into smaller grafts, both to be able cover a larger area of scalp and to generate enough 1-hair grafts for the frontal hairline. For the patient to benefit from this technique, the staff must thus be facile in stereo-microscopic dissection. Since dividing follicular units involves some potential risk to the viability of follicular unit grafts, the physician must decide the risk vs. reward benefit of this technique on a case-by-case basis.
Another thing to consider is the nature of the follicular units harvested. For example, a compact 3-hair FU should rarely be subdivided, whereas the patient who wears his hair short and has significant hair loss will almost always benefit from dividing loose, 4-hair units into two 2s, or dividing 5-hair “follicular unit families” into 3s and 2s. ((Seager D. Dense hair transplantation from sparse donor area – introducing the “follicular family unit.” Hair Transplant Forum Intl 1998; 8(1):21-23.)) In our practice, decisions on FU dissection are made based on the patient’s needs and real-time feedback during the dissection regarding the quality and composition of that patient’s grafts.
With the one-pass algorithm, the number of harvests per unit area is approximately 10-15% less than with random harvesting. With the two-pass algorithm, the number of harvests per unit area is about 5-8% less than with random harvesting.
The time required to process a grid is slightly increased when using the FU graft selection algorithm. With the two-pass algorithm, after the first pass, the robotic arm takes about 5 seconds to return to the start position for the second pass. In addition, the harvesting speed of the second pass is a bit slower, since the 1-hair grafts harvested during the second pass are more spread out and, therefore, the arm has a slightly further distance to travel between harvests. This adds an additional 10 seconds to an average grid. For a 2,000 grafts procedure (about 20 grids) the total additional time for the two-pass algorithm compared to the random harvesting of an equivalent number of grafts is about 5 minutes for the entire procedure [(5 seconds + 10 seconds) x 20 = 300 seconds].
Follicular Unit Graft selection will have the potential to deplete the donor area more rapidly than random graft selection. We have found that setting a minimum distance between harvests of 1.7mm insures that the area will not be over-harvested, regardless of the patient’s density and hair characteristics (as long as they are candidates for FUE). This distance is generally increased for the second hair transplant session, depending on how the patient looks clinically (we wait a year between sessions if the same area is accessed) and how short he wants to wear his hair. In our experience, a third session in the same area is generally not possible.
The data presented in this study is from the third iteration of this technology. Each modification has increased the specificity of the graft selection and further improvements are in progress. As the technology evolves, the clinical benefit of graft selection (i.e. the amount of hair yielded compared to the number of donor wounds made) should continue to increase.
Robotic FU graft selection allows the clinician two main capabilities: to maximize the hair content of the follicular units for specific cosmetic purposes that need high density (e.g. increased density of forelock) and to dissect these FUs microscopically to create a greater number of grafts using the minimal number of harvest attempts.
Since the introduction of robotic FUE in late 2011, a number of significant advances have been made in R-FUE technology. These include an improved optical system, refinements of the punch design, smaller punch sizes, faster punch rotation, a simplified user interface, and recipient site creation. ((Canales MG, Berman DA. The age of surgical robots. Hair Transplant Forum Intl. 2008; 18(3): 95-96.)), ((Bernstein RM, Rassman WR. Pre-making recipient sites to increase graft survival in manual and robotic FUE procedures. Hair Transplant Forum Intl. 2012; 22(4): 128-130. )), ((Bernstein RM, Wolfeld MB, Zingaretti G. Robotic recipient site creation in hair transplantation. Hair Transplant Forum Intl. 2014; 24(3): 95:97. )) Robotic follicular unit graft selection is another advance in the ever-evolving robotic system that continues to make the FUE procedure more accurate in the hands of clinicians and more beneficial to patients.
The algorithms used to perform the robotic functions used in this study were developed by Gabe Zingaretti, PhD at Restoration Robotics.
Statistical analysis was performed by Natalie J. Suder, Tulane University, New Orleans, Louisiana.
Disclosure: The investigators hold equity interest in Restoration Robotics, Inc. In addition, Dr. Bernstein is a medical consultant to the company and is on its medical advisory board.
The study was conducted at Bernstein Medical – Center for Hair Restoration in New York.