Robert M. Bernstein, M.D., William R. Rassman, M.D.
Hair Transplant Forum International 2006; 16(1): 229, 237-9.
When we published the technique of Follicular Unit Extraction (FUE) in 2002, Dr. Rassman and I described a two-step process for this new hair transplant procedure. ((Rassman WR, Bernstein RM, McClellan R, Jones R, et al. Follicular Unit Extraction: Minimally invasive surgery for hair transplantation. Dermatol Surg 2002; 28(8): 720-7.)) The first step was to use a sharp, circular instrument to separate the follicular units from the surrounding tissue and then to remove them from the scalp using fine forceps. The success of the hair restoration varied from patient to patient, so we developed a simple test (The FOX Test) to see which patients were good candidates for this type of procedure. Hair transplant patients that were FOX 1 had virtually no transection (damage) to follicles during their removal and those with lower FOX ratings exhibited more transection, with FOX 5 patients having excessive damage during the extraction.1, ((Bernstein RM, Rassman WR, Anderson KW: Follicular Unit Extraction Megasessions: Evolution of a technique. Hair Transplant Forum International 2004; 14(3): 97-99.))
The three-step technique for Follicular Unit Extraction (FUE) is based upon Dr. Harris’s concept of using a blunt instrument to prevent damage to follicles during the process of separating the follicular unit from the surrounding donor tissue. The three steps are: 1) scoring – using a sharp punch, 2) blunt dissection – using a dull instrument, and 3) extraction – using fine forceps. ((Harris JA. The SAFE System: New Instrumentation and Methodology to Improve Follicular Unit Extraction (FUE). Hair Transplant Forum Intl. 2004; 14(5): 157, 163-4.)), ((Rassman WR, Harris J, Bernstein RM. Follicular Unit Extraction. In Stough-Haber 2005 (Accepted for Publication). )) The three-step procedure decreased the amount of transaction in virtually all hair restoration patients and thus enabled a greater number to be classified as FOX 1. However, the three-step procedure introduced a new problem with FUE, that of buried grafts.4
Why Use a 3-Step Technique?
The need for the three-step procedure has two basic anatomic underpinnings (Figure 1). The first is that the angle of the hair that sticks out above the surface of the skin is not the same as the angle of the hair follicle below the skin’s surface. In addition, the angles differ from follicle to follicle. Therefore, it is literally impossible to exactly align the cutting instrument with the hair follicle as it passes into the depths of the dermis.
Figure 1. The anatomic features of the follicular unit that make blunt dissection important.
The second issue is that, although the follicles in the follicular units are gathered or grouped on the surface (Figure 2) and in the mid-dermis (Figure 3), as they sit deeper into the skin they spread outward so that by the time they enter the subcutaneous fat, they then become random (Figure 4). Therefore, a cutting instrument that easily fits around the follicular unit on the surface of the skin (Figure 2) will cut off the root of the follicles as it passes into the fat (Figure 4).
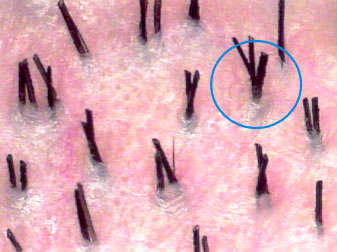 Figure 2. Follicular units well-demarcated on the surface of the scalp.
Figure 2. Follicular units well-demarcated on the surface of the scalp.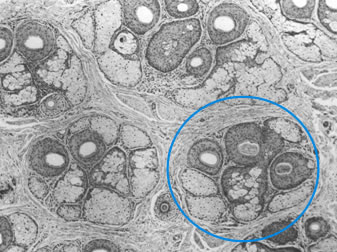
Figure 3. The punch fitting neatly around a 3-hair follicular unit at the level of the mid-dermis.

Figure 4. The punch transecting the bulbs of the follicles in the fat.
A solution to the problem is to use an instrument that would pass around the follicular units and essentially gather up the follicular bulbs that are spread out in the fat3. We used a prototype instrument that could be used for the blunt dissection step and we examined forty hair transplant patients in our study to confirm this hypothesis. We looked at twenty grafts extracted from the donor area of each patient. One side was done with two-step FUE and the opposite side with three-step FUE. Using a stereo-microscope at 10X, we evaluated the size of the follicular units and the amount of follicles lost through transection.
In interpreting the results, one first needs to define a few terms. The graft yield is simply the number of grafts versus the number of attempted extractions. This is actually a deceptive number because if you extract only one hair from a multi-haired follicular unit that would still be called a graft (this convention is used by many hair transplant doctors performing FUE). What is more valuable information is hair yield. The hair yield is the number of intact hairs obtained versus the total numbers of hairs in the follicular unit that one is attempting to extract. (Figure 5)
Figure 5. Defining graft yield and hair yield to accurately communicate the results of FUE.
As an example, in a case where only one intact hair was obtained from a 3-hair follicular unit, the graft yield would be 100 percent, whereas the hair yield (which is really the more important measurement) would be only 33 percent.
The results of this study showed that for the two-step technique the graft yield was reasonable, 92 percent, but the hair yield is only 74 percent. With the three-step procedure, it was 98 percent and 93 percent respectively, so there was a really significant improvement with the three-step technique in maintaining intact hair follicles. (Figure 6)
 Figure 6. Results of the study used to validate the advantages of 3-Step FUE.
Figure 6. Results of the study used to validate the advantages of 3-Step FUE.Although this three-step procedure is superior to a two-step procedure in avoiding follicular transection and in preserving follicular units, there was a greater incidence of buried grafts.
Buried Grafts
Buried grafts occur when grafts are inadvertently pushed into the subcutaneous tissue during FUE. These grafts can be left alone, but they may develop into cysts that would eventually need to be removed. If they’re not completely buried, the grafts can sometimes be extracted using a small instrument called a Shamberg extractor (the instrument used by dermatologists to remove black-heads). In the more common situation, you must extend the incision slightly so that the buried graft can be grasped with forceps. We use a No. 11 scalpel blade for the incision. Removing buried grafts, although not difficult, is extremely time-consuming. If one has a buried graft rate over a fraction of a percent, it becomes a significant logistical problem for the hair transplant surgery.
The incidence of buried grafts can be reduced by avoiding the nuchal area (the lower part of the scalp) where the angle of the hair is very acute and the skin has more resistance to the punch. Another trick is to clip the hair very short (less than 1-mm) before extracting, as a trapped hair will push the graft deeper into the scalp. One can also make the sharp cut slightly deeper and the dull dissection more superficial. On occasion, changing the angle of both the sharp and/or blunt instrument can minimize the incidence of buried grafts. Reverting back to a two-step procedure works well in select hair transplant patients, particularly those with very coarse hair. Finally, you can optimize the blunt tip design.
New Instrument Design
We looked at a number of different designs for the blunt-edged instrument. The first design we tried was a beveled edge. When beveling the edge inward, we found that the constricting lumen pushes down on the graft, so this clearly was not the answer. We tried placing the bevel on the outside surface, but the width of the wall was a problem with this configuration as well.
Going back basics, we tried a more simple design – a cylindrical tube. It was easy to make, the edge didn’t wear down, and it was reusable. The problem with a cylinder, however, was that the flat edge also pushed the grafts into the subcutaneous space. We tried to vary the wall thickness with the idea was that if the wall of a simple cylinder was thin enough; it could dissect the follicular unit from the surrounding tissue without pushing the grafts into the fat. The problem was that these instruments were too fragile.
We added a bull nose edge to one end of the cylinder with the idea that a rounded edge would make blunt dissection possible without the necessity of having to make the wall too thin. We used two techniques to create this rounded edge. One was an acid bevel (also called electro-polish) which made only a minor modification to the edge. The second, was the more conventional mechanical grind and polish. This turned out to be the technique of choice for the manufacturing of the tool.
The next step was to try to determine the appropriate internal and external diameter. We used a one-millimeter Miltex punch for the scoring step (the 1-mm Miltex punch is actually a 0.9mm OD punch). For the blunt dissection phase, we found that a larger punch would fit into the opening of the scored area, since the skin that was separated from the graft stretched to make the hole slightly wider.
We found an internal diameter of 1.37 mm to be optimal for the blunt instrument, as this fit nicely around the top of the scored follicular unit and could accommodate units of up to 4-hairs. With an outside diameter of 1.5mm, the instrument would have a wall width of 0.064mm (2.5 thousandths of an inch) that was thick enough to give the instrument stability, yet still small enough to fit into the wound. (Figures 7 and 8)
 Figure 7. The specifications of the Cylindrical Punch
Figure 7. The specifications of the Cylindrical Punch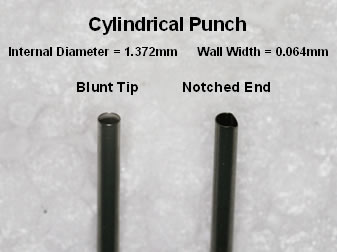 Figure 8. Detail of the two ends of the Cylindrical Punch
Figure 8. Detail of the two ends of the Cylindrical PunchWe inserted the notched end into a Versi handle with about seven millimeters of the blunt-tipped end exposed (Figure 9). One can shorten this end to 4- or 5-mm and use the handle as a “stop” i.e. a depth control, but it makes it slightly more difficult to control the angle.
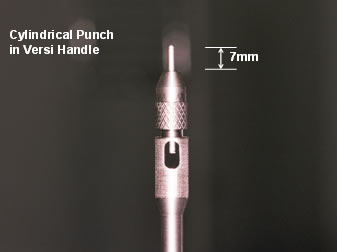 Figure 9. Cylindrical Punch in Versi-Handle.
Figure 9. Cylindrical Punch in Versi-Handle.We found that the incidence of buried grafts decreased significantly with the new instrument – from about 9 percent to 1.8 percent with the new device. However, we still found significant variability between hair restoration patients, making pre-procedure testing (Fox Test) still useful.
Conclusion
Performing Follicular Unit Extraction with a 3-step technique allows the hair restoration surgeon to minimize follicular transection and keep follicular units intact. A disadvantage of the 3-step technique over a 2-step process is the increased incidence of buried grafts. This can be reduced by modifying ones extraction techniques and using an instrument that is specifically designed to facilitate the blunt-dissection step of the process. The three-step technique, using customized instrumentation to avoid transection, is just one more step in the evolution and refinement of FUE.




