Robert M. Bernstein, MD, New York, NY and William R. Rassman, Los Angeles, CA
In: Haber RS, Stough DB, editors: Hair Transplantation, Chapter 12. Elsevier Saunders, 2006: 91-97. © 2006, Elsevier Inc.
Introduction
The underlying concept of follicular unit transplantation (FUT) is that, in order to maximize the cosmetic benefit of the hair restoration, only naturally occurring, individual follicular units (FUs) should be transplanted. In the purest form of FUT, FUs are neither divided into smaller units, nor combined into larger ones.
FUT had its origins in the microscopic dissection techniques of Limmer, developed in 1988. The conceptual framework for FUT was introduced in the hair transplant literature by the authors in their 1995 publication Follicular Transplantation and further detailed in 1997. The name follicular unit transplantation was formalized by a group of hair restoration surgeons in a 1998 publication in Dermatologic Surgery. In this paper, an attempt was made to precisely define FUT and included the two basic techniques of Limmer,single-strip harvesting and stereomicroscopic dissection, as integral parts of the procedure. Since FUs can now be harvested directly from the donor area without the necessity of a strip incision (using follicular unit extraction or FUE), the original definition of FUT has become obsolete. FUT is simply the transplantation of FUs by any means.
Other surgeons have regarded FUT as simply the transplantation of FUs by any means, thus a strict definition of this involving strip harvesting and stereomicroscopic dissection was never accepted by all. FUs can be produced by many methods, one of which is FUE. Transplantation of grafts obtained by FUE is still regarded as a form of FUT.
In order to transplant grafts in very high densities or in very large numbers per session, some practitioners have limited FUs to those containing a maximum of three hairs, particularly in those patients with coarse hair. This would necessitate dividing a naturally occurring four-hair FU into smaller grafts, essentially creating micrografts. Other practitioners of FUT occasionally combine two FUs with the intention of creating more density in the forelock area, particularly in patients with fine or light-colored hair. Other physicians may combine one-hair FUs into ‘twos’ simply to minimize the number of recipient sites needed. Finally, unlike strip harvesting with stereomicroscopes, where intact naturally occurring FUs are generated, for the vast majority of the time with FUE techniques the physician is not always able to harvest intact units and therefore must work with partial groups or groups devoid of some of the connective tissue support structures.
Considering these relatively common variations on FUT and the often imperfect FUs that are generated in the increasingly popular technique of FUE, FUT should be considered as any procedure in which the goal is to restore a person’s hair using predominantly naturally occurring individual FUs. It is important that where significant exceptions or deviations are made from the pure FUT procedure these modifications are clearly explained.
FUE may be considered a specific harvesting method in FUT in which FUs are obtained directly through small circular incisions rather than through a microscopically dissected donor strip. However, the nature of the technique itself can have a significant impact on other aspects of the surgery, including the quality of the grafts, their number, the organizational aspects of the surgery, and possibly its design.
Transplanting Individual FUs
There are two central arguments for transplanting individual FUs. The first is that using individual FUs will produce the most natural results. The second is that it allows the practitioner to transplant the maximum amount of hair into the smallest possible wound.
Natural Results
Since hair naturally grows as individual FUs, it is logical to conclude that transplanting hair exactly the way it grows would produce the most natural results. This apparently obvious conclusion however may not always be true. As will be discussed in a subsequent section, the normal density of FUs is approximately 100/cm2. If an average FU contains 2.3 hairs, there will be 230 hairs/cm2. In the context of this density, FUs of any size will look natural. However, if 2400 FUs are transplanted evenly over the front and top of a bald scalp (excluding the crown), an area that generally measures 150 cm2, the new transplanted density is 16 follicular units/cm2 or 16% of the original density. A second procedure of 2000 grafts, evenly distributed, will increase the average density to just under 30% of the original density. However, most physicians transplant greater densities toward the front part of the scalp (40–50%), leaving the area toward back of the scalp thinner. Therefore, even with two sessions totaling 4400 grafts, there may be as little as 20% of the original density on the top of the scalp and as little as 10% towards the back. If the crown is transplanted, these numbers will be even lower.
At low densities, there may not be enough hair to ‘visually support’ the larger FUs and four-hair grafts may have a slightly unnatural look. This may present a particular problem in patients with coarse, dark hair and light skin. One solution is to try and bury the larger units in areas of greater density, such as in the forelock area, and use the smaller grafts towards the periphery, but in patients with extreme skin/hair color contrast this may not be enough and it may be appropriate to split some of the four-hair units into two, two-hair grafts.
A second issue is that merely using individual FUs will not insure that the grafts look natural. The right-sized units must be placed in the right place. Since the normal hairline consists mainly of single-hair FUs, so must the transplant. This, however, is not always easy to do. Transplanting the naturally occurring FU implies keeping the support structures intact, which is best accomplished using a ‘chubby’ graft. Chubby grafts, however, increase the chance that empty telogen follicles are included in the dissection. Although this is beneficial to achieve maximum fullness for most of the scalp, at the hairline this may result in two-hair grafts. To avoid this problem, FUs at the hairline should be trimmed ‘thin,’ which may expose the graft to mechanical injury and desiccation.
Another problem occurs when small transplant sessions are performed. This may due to a demand issue (i.e. if the patient is a Norwood Class III and only requires 800 grafts) or a supply issue (i.e. if the patient can only afford a small number of grafts or FUE is planned and a limited number of grafts is a constraint due to the capabilities of the surgical team).
Since the normal donor scalp contains only around 10–15% one-hair FUs, a donor strip of 800 grafts would only yield 100–150 single-hair FUs, far short of the 250–300 generally needed for the frontal hairline.
In strip harvesting, if the surgeon desires to restore a hairline in one session then he or she must resort to splitting larger FUs into one-hair grafts. FUE presents another problem since harvesting single-hair FUs with this technique greatly increases the number of the recipient wounds. In FUE, in order to minimize injury to the donor area, it may be beneficial to harvest the largest FUs and then divide them into one-hair grafts for the hairline. This has been a common practice for over a decade among transplant surgeons and is a minor departure from pure FUT.
Small Wounds
That scalp hair grows in FUs, rather than individually, is most easily observed by densitometry, a simple technique where scalp hair is clipped to approximately 1 mm in length and observed through a high-magnification instrument (Fig. 12.1). From this vantage point, it can also be appreciated that follicular units are relatively compact, but are surrounded by substantial amounts of nonhair-bearing skin. The actual proportion of nonhair-bearing skin is probably about 50%, so that its inclusion in the dissection can have a substantial effect upon the outcome of the surgery. When multiple follicular units are used, and the skin is included, these effects are magnified.
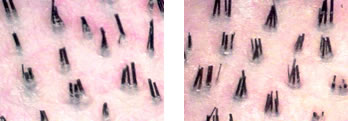 Figure 12.1. Densitometry showing discrete natural groups as the hair emerges from the scalp. These groups are the clinical correlate of the follicular unit. A) Slightly low donor hair density at 2.0/hairs per follicular unit. B) High donor hair density at 3.2/hairs per follicular unit. Both patients have the same follicular unit density of 1FU/cm2.
Figure 12.1. Densitometry showing discrete natural groups as the hair emerges from the scalp. These groups are the clinical correlate of the follicular unit. A) Slightly low donor hair density at 2.0/hairs per follicular unit. B) High donor hair density at 3.2/hairs per follicular unit. Both patients have the same follicular unit density of 1FU/cm2.The advantage of FUT over mini-micrografting and other grafting techniques is that in the former procedure the excess skin between FUs is trimmed away rather than transplanted. Therefore, a two-hair FU will consist of two closely spaced follicles and a single sheath of circumferential connective tissue. In contrast, a two-hair micrograft comprised of two distinct one-hair FUs will contain both the circumferential sheaths of each unit and the connective tissue between them, significantly increasing the bulk of the graft and the subsequent wound that must accommodate it (Fig. 12.2). The same argument can be made for grafts containing three or more hairs that are not pure FUs.
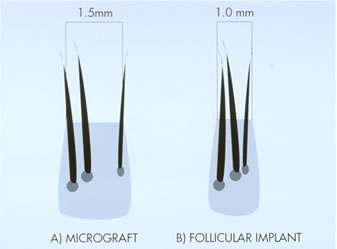 Figure 12.2 A) A 3-hair micro-graft. B) A 3-hair follicular unit. Note the much smaller volume the follicular unit compared to the corresponding micro-graft.
Figure 12.2 A) A 3-hair micro-graft. B) A 3-hair follicular unit. Note the much smaller volume the follicular unit compared to the corresponding micro-graft.A great benefit then, of using individual FUs, is that the wound size can be kept to a minimum, while the amount of hair that can be placed into it is maximized. Having the flexibility to place up to four hairs in a tiny recipient site has important implications for density, the design, and the overall cosmetic impact of the surgery.
The importance of minimizing the wound size cannot be overemphasized, particularly in larger hair transplant sessions or when grafts are densely packed. Larger wounds risk damage to the larger blood vessels in the scalp as well as disrupting the microcirculation. Poor recipient circulation increases the risk of postoperative infection, skin necrosis and poor or no hair growth. This is of particular concern when the blood supply to the scalp is already compromised from severe solar degeneration or chronic smoking, or when it is diminished from longstanding baldness.
The compact FU is, of course, the ideal way to permit the use of the smallest possible recipient wounds, and has made the transplantation of large numbers of grafts technically feasible. At times, however, when dense packing is taken to the extreme, such as when the goal is 50 or more grafts per cm2 in one session, even four-hair naturally occurring FUs may be too large for the surgeon’s needs. In this case, the largest FUs must be split in order to fit into arbitrarily small sites. Although these authors prefer to make the recipient sites slightly larger to accommodate the larger grafts, some surgeons performing very large sessions of densely packed grafts prefer to split the units to keeps the sites uniformly small.
Another important advantage of the small wound is a factor that can be referred to as the ‘snug fit.’ Unlike a punch, which removes recipient connective tissue, a small incision, made with a needle or similar fine instrument, retains the basic elasticity of the recipient site wall. When a properly fitted graft is inserted, the recipient site will then hold it snugly in place. For example, two- to three-hair FUs will fit snugly into 20 or 21 gauge needle sites, while single-hair FUs will fit nicely into 21 or 22 gauge needle sites, or into sites made with 0.6–0.7 mm rectangular blades. This ‘snug fit’ has several advantages. During surgery, it minimizes popping, and the need for the potentially damaging re-insertion of grafts. After the procedure, it ensures maximum contact of the implant with the surrounding tissue, so that oxygenation can be quickly re-established. In addition, by eliminating dead space, there is less coagulum formed and wound healing is facilitated. The time it takes after a transplant for grafts to be securely fixed in place can be shortened by as much as 4 days if a coagulum is not allowed to form.
Transplanting in Large Sessions
A main advantage of using FUs is that the small sites permit the transplantation of large numbers of grafts with minimal wounding. The advantage of transplanting in large sessions include: (1) social issues; (2) planning for telogen effluvium; (3) economizing the donor supply; and (4) flexibility in using different-sized FUs.
Social Issues
An obvious advantage of transplanting in large sessions is to achieve the patient’s objectives as quickly as possible with as little interference with their lifestyle. For patients who have hair loss through Norwood Class VI, the transplantation of 2400 FU grafts will provide coverage, albeit thin, from the frontal hairline to the vertex transition point (Fig. 12.3). It will give the patient a natural look after one session and if distributed properly will allow one procedure to stand on its own. A second session can be used to add density, but should not be required for the procedure to look natural, a goal that should be accomplished in the first session.
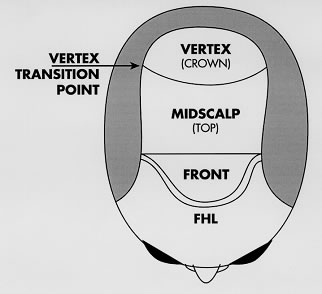 Figure 12.3 Regions of the scalp anterior to the vertex transition point.
Figure 12.3 Regions of the scalp anterior to the vertex transition point.Some physicians advocate a ‘one-pass’ procedure to achieve the final density. It is felt by proponents of the one-pass session that graft growth is maximum in a virgin area and, therefore, as much density as possible should be achieved in the first session. It is these authors’ opinion that if this goal leaves the patient with areas uncovered anterior to the vertex transition point, then it would be better to distribute the same number of grafts more broadly to produce a more natural distribution in the first session. It will also decrease the risks associated with very dense packing, namely graft popping and desiccation, insertion injury, and possible vascular compromise that may lead to poor growth. Poor growth associated with dense packing is of particular concern in longstanding baldness and in areas of significant solar damage, which alters the cutaneous vasculature.
Surgical Effluvium
Regardless of the technique, an inevitable aspect of hair transplant surgery is that the patient’s existing hair in and around the transplanted area has a chance of being shed as a result of the procedure. The hair that is at greatest risk of being lost is the hair that has already begun the process of miniaturization and if this hair is near the end of its lifespan, it may not return.
Often this shedding is mild and insignificant, but at times it can leave the patient with a thinner look after the procedure. Identifying those patients especially at risk by assessing increased levels of miniaturization, educating all patients that this process can occur, and planning for effluvium surgically are important aspects of the hair restoration process.
Performing large-transplant sessions are particularly useful if there are large areas of miniaturization that produce insufficient coverage and have not been responsive to finasteride and/or minoxidil. In these cases transplanting through (rather than around) an area that is highly miniaturized should be considered, since it is likely that this area will be lost by the time the transplant has grown in. An example would be to transplant through the ‘bridge’ of Norwood Class V patients who are beginning to show signs of breakdown.
The surgeon should plan to use enough FUs so that, if possible, the volume of transplanted hair is greater than the volume of hair that will likely be lost from surgical effluvium. In areas of extensive miniaturization, it may be appropriate to transplant FUs in the same density as if the area was totally bald.
Economizing Donor Supply
Regardless of how impeccable the surgical technique is, each time an incision is made in the donor area, and each time sutures are placed, hair follicles are damaged or destroyed. This damage can be minimized (but not eliminated), by keeping the sutures very close to the wound edges (so that they don’t encompass much hair), removing them early, and using nontension closures.
In addition, the healing distorts the direction of the hair follicles and increases the risk of transection in subsequent procedures. In subsequent procedures the damage can be reduced by using the previous scar as the upper or lower border of the new excision. In this way the amount of distortion and possible damage to existing hair is limited to only one free edge.
Another problem is that the fibrosis from the healed linear scar makes the scalp less mobile for subsequent surgeries, thus decreasing the amount of additional donor tissue that can be harvested. Each time there is surgery these factors come into play, therefore transplanting in large sessions, which minimizes the total number of individual procedures, will conserve total donor hair.
FUE techniques would seem to circumvent these problems; however, they also cause fibrosis of the donor area, limiting the yield in future surgeries. The extent to which present FUE procedures limit future ones is not yet known, but considering that FUE relies on secondary intention healing, the effects are likely to be significant.
Follicular Unit Sorting
In FUT the numbers of grafts present in any given size donor strip is determined by nature, since each graft represents one FU. It follows that if only the naturally occurring individual units are to be used, practitioners are limited by their normal distribution in the scalp (Fig. 12.4). Using larger sessions, greater numbers of each type of unit will be generated, adding flexibility to the surgery. This will enhance the cosmetic outcome of the procedure when the surgeon seeks to create soft transition zones using single-hair units or when creating central density with three- and four-hair FU grafts.
 Figure 12.4 Distribution of follicular units in the scalp in patient with low, average and high hair densities. This would correspond to the graft yield using stereo-microscopic dissection.
Figure 12.4 Distribution of follicular units in the scalp in patient with low, average and high hair densities. This would correspond to the graft yield using stereo-microscopic dissection.Clinical Characteristics of FUs
FU Constant
One of the interesting aspects of transplanting with FUs is that nature was kind to space them at approximately one per mm2. This has been observed clinically using densitometry and stereomicroscopic dissection and histologically using transverse microscopic sections of the skin (this was first described by Headington in 1984). Not only does a FU constant of 1 unit/mm2 make the math easy, but it makes accurately estimating the donor harvest possible, and gives a logical basis for planning the density and distribution of the grafts.
The constancy of FU density has been studied, but inconsistent study designs prevent accurate conclusions. There is general agreement on the following:
1. FU density generally decreases as work moves laterally from the mid-occiput at the level of the occipital protuberance towards the temples.
2. FU density varies among races such that the darker skinned races tend to have the lowest FU densities and light-skinned races the highest (Table 12.1).
3. Within the same race and same location on the scalp, there is significant person-to-person variation in FU density.
4. Given points 1–3 above, the constancy of the FU density is still rather striking so that patients with high hair density have more hairs per FU rather than FUs spaced closer together and those with low hair density for the most part have fewer hairs per FU than units spread further apart (Fig. 12.1).
Although the FU density is not exactly 1/mm2, it is close enough to this number that it can be extremely useful in the surgery. Once it is realized that the FU density is relatively constant and that hair density varies, it follows that the number of hairs per follicular unit largely determines hair density. The implications of this in hair transplantation can be summarized as follows:
- Since the FU density is relatively constant, the same number of FUs should generally be used to cover a specific-sized bald area regardless of the hair density of the patient.
- With low hair density, using the same number and spacing of FUs as in a patient with high density will help to ensure that there is proper conservation of donor hair for the long term.
- Hair density is a characteristic of the FU specific to each individual, and together with hair shaft diameter, color and wave, will determine the cosmetic impact of the transplant.
Hair Characteristics
The results of a hair transplantation procedure are determined as much by the characteristics of the individual hairs as the number of hairs per FU. Since hair counts are easily measurable, the more subjective hair characteristics, or the ones more difficult to measure, are often discounted. Many characteristics including hair shaft diameter, hair color, texture (wave, curl, kink) and other factors such as the emergent angle of the hair, static, oiliness, or sheen, all contribute to the appearance of fullness, however, hair shaft diameter probably has the greatest impact.
The total volume of hair determines the visual impact. Doubling the hair density doubles the hair volume, while doubling the hair diameter quadruples the hair volume (remember ?r2). Hair density varies from 1.5–3.0 hairs/mm2, while hair shaft diameter varies from 0.06–0.14 mm. Therefore, hair shaft diameter plays a greater role than absolute hair numbers in determining overall cosmetic impact (Table 12.2).
Conclusion
The introduction of FUT created a literal revolution in hair restoration surgery, with doctors discarding their multi-bladed knives, buying stereomicroscopes, and training their staff in the dissection of individual FUs. However, the belief that in order to get the best results, only naturally occurring individual FUs should be transplanted has not been universally accepted.
With the new harvesting method of extracting FUs directly from the donor area, new technical issues are challenging the wisdom of always keeping FUs intact. In particular, if the object is to minimize the number of recipient wounds when performing FUE, it may pay to split larger units into single hairs to create a soft hairline rather than making separate punch holes to harvest each one-hair graft. This and other technical issues of FUE, where only partial units are removed, require fresh thinking about what should constitute FU transplantation.
Editors’ Note
This chapter succinctly outlines the importance of the FUs. Many of the concerns raised in this chapter over the use of magnification and transplanting only intact FUs pertain to the Caucasian population. Transplant surgeons who operate primarily on Asians and those of middle-eastern descent have not found the requirement for stereomicroscopic magnification absolute. These surgeons have also routinely divided FUs in order to achieve more single-hair grafts in the frontal hairline.
Further Reading
Bernstein RM, Rassman WR 1997 Follicular transplantation: Patient evaluation and surgical planning. Dermatologic Surgery 23:771–784
Bernstein RM, Rassman WR 1997 The aesthetics of follicular transplantation. Dermatologic Surgery 23:785–799
Bernstein RM, Rassman WR 1999 The logic of follicular unit transplantation. Dermatologic Clinics 17:277–295
Bernstein RM, Rassman WR, Seager D, et al 1998 Standardizing the classification and description of follicular unit transplantation and mini-micrografting techniques. Dermatologic Surgery 24:957–963
Bernstein RM, Rassman WR, Szaniawski W, Halperin A 1995 Follicular transplantation. International Journal of Aesthetic and Restorative Surgery 3:119–132
Limmer BL 1994 Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation. Dermatologic Surgery 20:789–793
Rassman WR, Bernstein RM, McClellan R, Jones R, et al 2002 Follicular unit extraction: Minimally invasive surgery for hair transplantation. Dermatologic Surgery 28:720–727




