Pages:
&after=
&link_before=&link_after=‘); ?>
PLANNING THE HAIR RESTORATION
The two key aesthetic landmarks are the frontal hairline and the vertex transition point. In a mature adult, the mid-portion of the frontal hairline rests approximately one finger-breadth (1.5-2 cm) above the upper brow crease and is the position to which most hairlines should be restored. One should generally not place the hairline at the level of the upper brow crease, since this is the position of the adolescent hairline and will be too far forward as the patient ages. The hairline should recede towards the temples, but there is more flexibility in designing the hairline at this location.4
The vertex transition point (VTP) separates the top of the scalp from the crown and is the most important posterior landmark to be considered when designing the hair transplant. The VTP is the point were the hair transitions from a predominately forward direction to form the radially oriented crown whorl.20 Stopping at this point will allow the transplant to look natural even if the patient becomes extensively bald and no further hair restoration procedures are performed. Fortunately, most people will have enough donor hair to reach this point. Extending the transplant beyond the vertex transition point should be reserved for hair transplantation patients with an above average donor supply. (Figure 5A, B)21
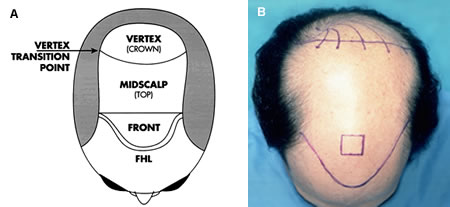 Figure 5A. Schematic of the regions of the scalp. The Vertex Transition Point is the part of the scalp where the hair changes from a predominantly forward direction to form the whorl. Figure 5B. Regions of the scalp. Note the predominately forward direction of hair markings as one crosses over the vertex transition point anteriorly.
Figure 5A. Schematic of the regions of the scalp. The Vertex Transition Point is the part of the scalp where the hair changes from a predominantly forward direction to form the whorl. Figure 5B. Regions of the scalp. Note the predominately forward direction of hair markings as one crosses over the vertex transition point anteriorly.In the first hair transplant session, the frontal hairline should be established and coverage should extend at least to the vertex transition point. Subsequent sessions should be used to achieve greater density or to address additional areas of hair loss.4 In general, the goals should be achieved in as few hair restoration sessions as possible to minimize the number of times the donor area is accessed and be the least disruptive to the patient’s life.
With the exclusive use of follicular units and concomitant use of small recipient sites, the risk of vascular compromise in the recipient area is small, even with large sessions. That said, large sessions cannot be performed with impunity. In general, we recommend densities in the range of 20-25 follicular unit/cm2 when large sessions are performed. Some hair transplant doctors advocate the use of higher densities, particularly in virgin scalps; however, it is our view that this may increase the risk of vascular compromise, graft popping, desiccation and other problems that can adversely affect graft survival. Transplanting large number of grafts also increases the time the grafts remain outside the body and creates more demands on the staff, both in technical skills and in organization. Large hair restoration sessions should not be performed by inexperienced physicians or those with limited surgical teams.4
Two important factors that affect the number and density at which grafts should be placed are photo damage of the recipient skin and smoking. Most doctors caution on photo-protection after hair transplant surgery, but give little attention to the effects of existing sun damage on the procedure. It has been this author’s personal observation that ultraviolet radiation alters the cutaneous vasculature so that the donor area is less able to support densely packed grafts. UV light also alters the collagen and elastic tissue so that grafts are held less securely. These factors need to be examined in well-controlled studies. The deleterious effects of smoking on wound healing have been well documented and the surgical planning in chronic smokers should be more conservative with respect to the density and the absolute numbers of grafts planted.22
Table 1 gives the recommended number of follicular unit grafts for the first hair restoration session organized according to the person’s Norwood class.2
The second session should be planned no sooner than 8-12 months after the first session, since it takes this amount of time for the hair from the first session to grow and for the cosmetic impact to be appreciated. Once the transplanted hair has reached its full length, diameter, and texture, the physician and patient will be in the best position to decide on the placement of additional grafts. Waiting to perform the second hair transplant will also allow donor laxity to return, although it rarely goes back to its original state. Finally, if there is significant Telogen effluvium after surgery, it may take up to a year for that hair to regrow.
The second session is used to add density to areas transplanted in the first session and to add coverage to any additional areas of hair loss. During the second session, it is often helpful to refine the hairline, usually by making it more irregular. Extending the transplant into the crown might also be considered in the second session if the first procedure produced adequate coverage in the area anterior to the vertex transition point and if there are adequate donor reserves.
Generally, the restoration can be completed in two sessions. Additional sessions reserved for addressing further hair loss. The total number of graft needed for a complete hair restoration is indicated in Table 2.3
PATIENT PREPARATION
Besides its role in hair regrowth, or in retarding the progression of hair loss, finasteride is often prescribed pre-operatively to minimize the chance of post-surgical shedding. However reasonable this practice, there is currently little scientific data to support this use or to indicate how far in advance of surgery the drug should be given. Patients using topical minoxidil should discontinue the medication several days before surgery (because it is a vasodilator and may increase bleeding) and wait until a week after the procedure before resuming it (to avoid the irritating effects of its alcohol/propylene glycol base). If a patient has been on minoxidil for an extended period of time and does not plan to continue the medication after surgery, he should stop the medication several months prior to the procedure. In this way, if there is significant hair loss, it may be accounted for in the surgical planning. On most hair transplant patients, finasteride should be continued long-term to help retard further balding.
To prevent damage to the grafts, patients who wear hair pieces should convert them to a tape-less, glue-less clip-on system that can easily be removed before showering and sleeping. The front edge of the piece can be kept in place with a stiffening-rod. Patients are encouraged to permanently discontinue the system after the procedure, but those who feel the need to use them until their hair grows in should wait at least five days post-op before wearing them and to use them as infrequently as possible.
Systemic antibiotics are not indicated for routine use in hair transplants. For those with a history of endocarditis or mitral valve prolapse, one should refer to the review by Haas and Grekin regarding antibiotic prophylaxis and consult with the patient’s primary physician.24 In the peri-operative period, patients should, of course, abstain from smoking, alcohol and medications that will increase bleeding. There is no consensus on the necessity of routine blood testing before hair transplantation.
The morning of surgery patients are advised to shampoo with chlorhexidine and wear a button-down shirt. In the office, patients change into a cotton surgical gown and are photographed from the neck up, with front, top and occasionally three-quarter views. The hairline and, if appropriate, the vertex transition point and crown swirl are marked in gentian violet and additional photos are taken. All photographs (or their digital counterparts) are kept as part of patients’ permanent medical record.
If there are no contraindications, patients who are not driving home after the hair restoration procedure, are pre-medicated with diazepam 15 mg PO (adjusted for body weight) and an intramuscular injection of methylprednisolone 80 mg.
SURGICAL TECHNIQUES
OR Setup
The dissecting stereo-microscope is the most important tool for performing follicular unit transplantation.1,9,24 There should be one microscope for each dissector at work stations with comfortable seating. Because the patient will be sitting for long periods of time, and the physician and staff will be working predominately on the top of the patient’s scalp, the operating tables should provide lumbar support when patients are sitting and need to be low to the ground (the seat surface should be 22 inches from the floor). Bright fluorescent ceiling lights generate less heat than high intensity OR lights and minimize bleeding during the hair transplant surgery.
Grafts should be stored on a stable surface, such as a counter top, that cannot inadvertently be knocked over. Grafts should be held in chilled normal saline or Lactated Ringer’s and the solution should be kept on ice blocks or refrigerated. Limmer has shown a high survival rate for grafts kept in chilled saline up to eight hours.25 To eliminate inadvertently placing grafts in the wrong patient, a small refrigerator for the grafts should be dedicated to each operating room.
Preparing for the Donor Harvest
With the patient in an upright position, the hair in the donor area is trimmed to 1-2 mm using electric clippers. The hair should be cut so that the center of the shaved area is at the level of the occipital protuberance and extends laterally over the ears. When harvesting a 1 cm wide strip, several millimeters should be trimmed on either side to facilitate suturing.
In calculating the strip length for Caucasian patients, it can be assumed that each 1 cm2 of donor tissue will yield approximately 100 follicular units.6 The yield will be less in dark-skinned races whose follicular unit density is slightly lower.4 The density will decrease in subsequent sessions and will be even less if all, or part, of the first donor scar is incorporated into the next incision. It is important to adjust the size of the strip accordingly.
Local Anesthesia
Local anesthesia is administered with a ring-block consisting of 60% lidocaine 0.5%, and 40% bupivacaine 0.025% with epinephrine 1:200,000 added to this mixture. Lidocaine is used for its safety and quick onset. Marcaine is used to increase the duration of anesthesia, but in smaller quantities to limit its potential cardiac toxicity.26 Epinephrine increases the anesthetic duration while decreasing its toxicity and providing some hemostasis. Its short-lived vasoconstrictive properties limit its usefulness in long hair restoration procedures.27 Sodium bicarbonate 8.4%, 1:20 is added to bring the acidic pH of the epinephrine containing solution closer to 7.4, to lessen its sting.28
In the donor area, the anesthetic solution is injected into the deep subcutaneous fat layer, approximately 1 cm below the lower portion of the clipped area and extending several centimeters past it on either side. On the forehead, the anesthesia must be injected into the superficial dermis as well as the subcutaneous space to insure its effectiveness. It is important to avoid injecting anesthetic into the muscle, as epinephrine will cause vasodilatation (due to the action on ß2-receptors), quickly dissipating the local effects of the anesthetic and increasing its toxicity.29
After the area is anesthetized, additional tumescent anesthesia is administered by injecting larger quantities of a more dilute solution of lidocaine (0.17%) and epinephrine (1:600,000) into the mid-fat to indurate the area. The tumescence serves to: 1) increase the distance from the follicles (residing in the upper fat) to the nerves and larger blood vessels (lying just above the fascia), 2) increase the rigidity of the donor area (that helps to decrease follicular transection during the harvest), 4) decrease bleeding, 5) produce more uniform anesthesia and 6) reduce the total amount of anesthetic required.
Single Strip Harvesting
When possible, the donor hair should be harvested as a single strip to minimize follicular transection. This can be accomplished with two parallel #10 blades set on a handle to cut the body of the strip, and then one blade used free-hand to taper the ends (we use the Rassman handle that angles the blades at 300 so that they are parallel to the emergent hair). Alternatively, the entire strip can be removed with an elongated free-hand ellipse.1 In a hair transplant patient with average scalp laxity, we generally harvest a donor strip that is 1 cm wide in the first session. It is important to plan the width of donor strip so that there is little or no tension on closure. (Figure 6)
 Figure 6. Single strip harvesting showing dissection in the subcutaneous plane using a #10 blade after the edges have been cut with two parallel blades on a Rassman handle.
Figure 6. Single strip harvesting showing dissection in the subcutaneous plane using a #10 blade after the edges have been cut with two parallel blades on a Rassman handle.An advantage of the free-hand method is that it allows the angle of the blade to be adjusted as each edge is cut. This technique, however, makes it harder to keep the width uniform; a prerequisite for predictable graft yields. Cutting the second edge also becomes more problematic since the tumescence is lost after the first incision and the tissue becomes more mobile.
As mentioned, the ideal location for the donor incision is in the mid-portion of the permanent zone that lies, in most people, at the level of the external occipital protuberance and the superior nuchal line. The muscles of the neck insert into the inferior portion of this ridge, so an incision below this anatomic landmark will be affected by the underlying muscle movement. A stretched scar in this location is extremely difficult to repair and re-excision risks an even wider defect. The main problems of harvesting hair too high on the posterior scalp are lack of permanence of the transplanted hair (since it may be subject to androgenic change) and future visibility of the scar with further hair loss.
In subsequent hair restoration procedures, the new incision can incorporate all, or part, of the old scar or a totally new area can be accessed. The argument for a single incision is that in this method, the hair is always harvested from the mid-portion of the donor zone where the shaft has the widest diameter (producing the most fullness), the density is the greatest (necessitating the smallest incision) and the hair will have the greatest likelihood of being permanent. Those in favor of multiple incisions point out that the hair yield will be greater if the old scar is avoided and feel that there is a smaller risk of a widened scar. This multiple strip technique, however, often necessitates making incisions at the outer margins of the permanent zones.
Donor Closure
The donor wound can be closed with a variety of suture materials and techniques.30,31 We prefer closing the donor wound with a running 5-0 suture made of the absorbable material poliglecaprone 25.32 Absorbable sutures can be placed very close to the wound edges (1.5 mm) without the concern that they become buried. Placing sutures close to the wound edge minimizes entrapment and destruction of follicles, particularly if there is significant post-op edema that increased tension on the closure. To further limit damage to follicles, the suture loops should be spaced approximately 4.5 mm apart and the stitch should be advanced on the surface of the skin to minimize the amount of suture in contact with the follicles. (Figure 7, 8)
Possibly the most common closure is a running stitch using with nylon or polypropylene. These sutures can be used with or without interrupted subcutaneous sutures. The advantage of using subcutaneous sutures in this instance is that is allows the cutaneous stitches to be placed loosely and removed early, minimizing follicular damage.
Staples are useful in hair transplantation because they have virtually no tissue reactivity; however, they make apposition of wound edges difficult. They are also uncomfortable and not tolerated well by the patient. We have found that staples, more often than sutures, result in a stretched scar, due to the difficulty in closely opposing the wound edges and are more likely to leave a scar that is visibly linear. For these reasons we prefer absorbable sutures, although staples may be particularly useful in patients with high density and very loose scalps.32
Follicular Unit Extraction
Individual follicular units can be harvested directly from the donor area, without the need for a linear incision, through a technique called Follicular Unit Extraction (FUE). In this procedure, a 1-mm punch is used to make a small circular incision around the upper part of the follicular unit, which is then extracted from the scalp.14,15
 Figure 7. Schematic of suturing technique. The heavy, diagonal line represents suture on the skin surface. The light, vertical line represents suture advanced in the sub-cutaneous space.
Figure 7. Schematic of suturing technique. The heavy, diagonal line represents suture on the skin surface. The light, vertical line represents suture advanced in the sub-cutaneous space.Because FUE does not leave a linear scar, it is appropriate for patients who want to wear their hair very short. The procedure is also useful in patients who have healed poorly from traditional harvesting or who have a very tight scalp. Possibly the most important application of this technique is to camouflage a widened linear donor scar from a prior hair transplant procedure.
 Figure 8. Suturing technique showing suture placement within 1.5mm of wound edge.
Figure 8. Suturing technique showing suture placement within 1.5mm of wound edge.Patients differ significantly with respect to the ease in which the units can be extracted from the scalp, with extraction in some patients producing unacceptable levels of transection. Not being able to have three or more persons working in parallel, as with microscopic dissection, is another disadvantage of this technique.
FUE’s main limitation is that it is less efficient in harvesting hair than follicular unit transplantation. In FUE, the defects remain open to heal by secondary intention and this causes significant scarring in the donor area. Although not clinically apparent, the scarring distorts follicular units adjacent to the harvested sites and makes subsequent sessions more difficult. In FUE, since a significant amount of intervening hair is left behind, a much larger region must be accessed to harvest the necessary amount of donor hair (compared to FUT). This forces the surgeon to eventually harvest hair from the inferior and superior margins of the traditional donor area and risks the hair being non-permanent.
All hair restoration patients considering FUE should be tested for the ease of extraction (the FOX Test)2 so that those who show significant degrees of transection can be identified in advance as non-candidates. Patients undergoing follicular unit hair transplantation should also be tested for follicular unit extraction at the time of surgery, in the event FUE may be useful in a future session. One such use might be the camouflage of the linear scar after the patient’s final FUT procedure.
Graft Dissection
In single-strip harvesting, the excised donor strip is first divided, under stereo-microscopic control, into thin sections taking care to avoid transection of follicles or dividing follicular units. This process, called “slivering” is generally performed in one of two ways.33 In the first, the larger strip is cut into very thin sections measuring only one follicular unit (1-mm) wide. In the second method, slightly wider sections (2-2.5 mm) are generated from the strip. These authors prefer the second method as we feel this technique makes it easier to keep the follicular units intact and generates a higher hair per follicular unit yield.
In either method, the strip is oriented on a water-soaked tongue-depressor blade with the hair pointing away from the dissector and the convex surface of the strip facing upward. One end of the strip is held with rat-toothed forceps by the person performing the slivering and the other end by an assistant to stabilize the strip. Some hair transplant doctors obviate the need for a second person by pinning the free end of the strip to the dissecting board. The slivering is carried out using a #10 blade on a #3 blade handle. The dissector begins to cut through the width of the strip, guiding the blade between follicular units and slivering in a one-directional fillet-like movement from the epidermal side to the subcutaneous surface. A back-and-forth sawing motion will cause unnecessary damage to the follicles (Figure 9).
 Figure 9. A donor strip is divided into thin sections in a process called “slivering.” In slivering, the scalpel blade passes around follicular units as it cuts through the strip to avoid damage to the follicular structures and to keep the units intact. The free end of the strip is stabilized by an assistant.
Figure 9. A donor strip is divided into thin sections in a process called “slivering.” In slivering, the scalpel blade passes around follicular units as it cuts through the strip to avoid damage to the follicular structures and to keep the units intact. The free end of the strip is stabilized by an assistant.Once the strip is divided into either 1-mm or 2-2.5mm slivers, the slivers are placed on their sides, stabilized with straight jeweler’s forceps, and then dissected under the stereo-microscope into individual one- to four-hair follicular units (Figure 10, 11).
 Figure 10. The slivers are dissected into individual follicular units.
Figure 10. The slivers are dissected into individual follicular units. Figure 11. One, two, three and four-hair follicular units.
Figure 11. One, two, three and four-hair follicular units.As the follicular units are isolated, they are sorted according to the number of hairs they contain, and placed into Ringer’s lactate filled Petri dishes set on ice blocks. When the several hundred grafts have been dissected, they are put into plastic specimen containers and refrigerated. All slivers and dissected follicular units should be bathed, at all times, in chilled Ringer’s lactate. It is convenient to keep 10-cc syringes containing Ringer’s lactate by each cutting surface for this purpose.
Creating Recipient Sites
In follicular unit transplantation, the tools used to create recipient sites should not remove tissue, i.e. one should not use a punch or trephine, as this causes unnecessary destruction of the recipient area. The most important factor in determining which instrument to use is the diameter of the wound they create. A number of other factors, including the shape of the tip (spear or lancet) and whether they are solid core or hollow, have some impact on the hair transplant surgery.34 Common hypodermic needles are used by many practitioners. Although a discussion of the different types of instruments is beyond the scope of this writing, as a general guide; the equivalent of 20-g needles can be used for one-hair follicular units, 19-g needles for two-hair and thin 3-hair follicular units, and 18-g needles for three- and four-hair follicular units. In special situations, such as using individual hair for eyebrow restoration, finer needles may be appropriate. In patients of African decent with very kinky hair, one hair units will often require at least a 19-g needle and 2-hair grafts an 18g needle.
Although it is best to keep recipient sites small to minimize wounding of the recipient area, this should not be at the expense of the grafts. None of the recipient sites produced by hypodermic needles of 18-gauge diameters, or less, will produce a visible scar, so one should not use a recipient site so small that the graft must be forcibly inserted. One must also balance the advantage of keeping follicular unit grafts “chubby” to preserve telogen follicles and create more insulation for the individual follicles (to prevent mechanical injury and desiccation) with the desire to make sites very small so that the grafts may be more densely packed.
There are two schools of thought with regard to making the recipient sites and inserting the grafts; pre-making the sites and the “stick and place method.” Pre-making all the recipient sites prior to graft insertion allows the physician to design the transplant and concentrate on angling and distribution without having to worry about the handling of grafts or their subsequent popping as additional sites are made. The actual creation of sites initiates coagulation so that when the grafts are placed there is little bleeding and no need for additional epinephrine. This allows for maximum visibility in the placing phase of the hair restoration procedure.35 The problem of matching the number of sites to the number of grafts can be solved by making mathematical projections of the anticipated number of grafts while the dissection is still in progress.
In the stick and place method, the grafts are inserted as the sites are made.33 In this technique, the needle can actually be used as a shoehorn facilitating the insertion of the grafts. The advantage of this method is that it eliminates the problem of leaving sites unfilled and avoids the risk of placing two grafts in one site (“piggybacking”). On the other hand, it increases the risk of popping (since a new site is made next to a site containing a graft), it forces the staff to focus on the technical aspects of graft insertion at the same time they must concentrate on design elements (such as angling and distribution) and it leaves many of the aesthetic decisions in the hands of the technicians performing the stick and place, rather than the physician.
POSTOPERATIVE CARE
After the grafts have been inserted, the scalp should be cleaned with distilled water to remove any residual blood. It is best to avoid using peroxide (even diluted) once the grafts have been placed. A final check is made to settle any grafts that are elevated. An antibiotic is applied to the sutures and a head-band type pressure dressing is placed over the donor area. The transplanted area is covered with a surgeon’s cap. Patients are given oral sedatives and pain medication, but if they have taken them during the procedure they are not permitted to drive home after the surgery.
Because the donor area is closed with absorbable sutures, patients do not need to return to the office for their removal; however, patients that live close to the office are seen a week after their procedure. Patients are seen again 8-12 months post-op to discuss their results and the possibility of additional hair transplant surgery.
Patients are instructed to shampoo every three hours the day following surgery and twice daily for the next week. The purpose of the frequent showering the day following the procedure is to minimize crusting. Once the crusts adhere to the hair shaft they will be difficult to remove and may pose a cosmetic problem for several weeks. They also make the transplanted grafts less secure. The reason is that, although hair will dissociate from the transplanted grafts around 4 days post-op, crusts that have adhered to the epidermal surface of the grafts can cause them to dislodge if they are picked, or scratched, for up to 8 days following the hair restoration procedure.
Patients are advised to avoid exercises that flex the neck and stretch the sutured donor wound. The length of time a patient needs to be careful depends upon the tension at closure and the length of the incision. Since policapterone 25 absorbable sutures loose their tensile strength in about three weeks, care should be taken for at least 4-6 weeks post-op. Photo-protection is advised for three months following the procedure and patient are instructed to avoid alcohol for a week and smoking for at least two weeks following surgery. If the patient chooses to continue Minoxidil after the procedure, it may be resumed in one to two weeks, as long as it doesn’t cause scalp irritation.
Pages:
&after=
&link_before=&link_after=‘); ?>




