Robert M. Bernstein, M.D.,*† William R. Rassman, M.D., ‡ Nazia Rashid, and Richard C. Shiell, M.B.B.S.
Dermatologic Surgery 2002; 28(9): 783-94.
*College of Physicians and Surgeons, Columbia University, New York, New York
†New Hair Institute Medical Group, A Professional Corporation, New York, New York and ‡Los Angeles, CA
© 2002 The American Society for Dermatologic Surgery
This is the first of a two-part series. Part I discusses the most common problems encountered in surgical hair restoration and presents general concepts in corrective work. Part II addresses the technical aspects of performing the actual restoration.
PART I: General Aspects of Repair and Basic Repair Strategies
Introduction to repair
Cosmetic problems produced by poorly executed hair transplants
Major limitations inherent in restorative procedures
Basic repair strategies
PART II: The Tactics of Repair
Why Follicular Unit Transplantation is the ideal tool for repair
Specific repair techniques
Removal and re-implantation
Removal alone
Camouflage
Special cosmetic problems
Repair of the donor area
When hair restoration surgery is performed on a “virgin” scalp, the goal is to mimic nature as closely as possible. This is accomplished by carefully matching the newly transplanted hair to the patient’s original hair distribution and growth patterns. Follicular Unit Transplantation, the technique that allows the surgeon to transplant hair exclusively in its naturally occurring groups of 1-4 hairs, represents the “state-of the-art” in this technology. ((Limmer BL. Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation. Dermatol Surg 1994; 20:789-793.)), ((Bernstein RM, Rassman WR, Szaniawski W, Halperin A. Follicular Transplantation. International Journal of Aesthetic and Restorative Surgery 1995; 3:119-132.)), ((Bernstein RM, Rassman WR. Follicular Transplantation: Patient evaluation and surgical planning. Dermatol Surg 1997; 23:771-784.)), ((Bernstein RM, Rassman WR. The aesthetics of Follicular Transplantation. Dermatol Surg 1997; 23:785-799.)) One of the major challenges of repair work is that the surgeon must start with a scalp that has been altered by surgery and make it appear natural. Under such circumstances, directly mimicking nature may not be possible.
Hair transplantation performed on a virgin scalp is a technique grounded in science. Artistic interpretations imposed by the physician can cause the results to deviate from the patterns created by nature. The successful hair transplant surgeon must, therefore, carefully observe nature and then copy it as best he can. In contrast, repair work is more of an “art.” Improperly performed hair restoration surgery presents a series of unique problems that are best solved by deviating from the normal rules that one would apply to a scalp free from prior hair transplant surgeries.
In repair procedures, the surgeon characteristically encounters multiple cosmetic problems in the same patient. Even more problematic, the improper techniques that caused the cosmetic defects are often the very same ones that limit the repair. Fundamental to all repair work is the establishment of a series of carefully prioritized goals so that if not all of the goals can be met, those most critical to the patient’s appearance will have been achieved.
The patient who has had a negative hair transplant experience is often depressed, angry, and distrusting. He presents the surgeon with a host of challenges that are not all surgical. The physician must restore confidence in the patient who feels betrayed by the medical community. He must establish trust in a patient who had been misled, set new goals when previous goals had not been met, and explain a sequence of new procedures when the prior ones were not well understood. He must provide hope to a person who wishes that he had never started the hair restoration process in the first place.
The doctor must educate his patient and support him as he embarks on a new series of surgeries with the understanding that the full benefits may not be immediately apparent. He must plan the surgery in concert with the social needs of the patient, and design the procedures so that specific styling and grooming techniques can work to enhance the surgical results. The doctor must then perform surgery with techniques individualized for the particular patient and handle problems that cannot always be anticipated before the surgery starts. Restorative work is thus a creative endeavor that combines communicative, surgical and aesthetic skills to achieve the patient’s goals. The process is truly an “art.”
A significant part of the hair restoration surgery performed in many referral practices involves some type of corrective procedures to fix poorly executed hair transplants, scalp reductions and flaps. ((Bernstein RM, Rassman WR. The logic of Follicular Unit Transplantation. Dermatol Clin 1999; 17 (2):277-295.)), ((Bernstein RM. Are scalp reductions still indicated? Hair Transplant Forum Intl. 1996; 6(3):12-13.)) Because of this, the skill and judgment involved in repair work are as essential to a practice as the ability to operate on a “virgin scalp.” Although many of the problems encountered today result from procedures that were routinely performed prior to the advent of the use of small grafts, the availability of “modern techniques” alone does not protect the patient against bad or antiquated work. Errors in surgical decisions, poor aesthetic judgments, operating on patients with unrealistic expectations, and performing procedures on patients who are not good candidates for hair transplantation, remain major problems.
Although the use of very small grafts, and now follicular units, eliminates many of the more blatant problems associated with the older procedures, there are new “cost cutting” techniques used by some physicians that present new areas of concern. ((Bernstein RM. Blind graft production: Value at what cost? Hair Transplant Forum International 1998; 8(6):28-29.)) The lure of these techniques is that they appear to save the patient money with relatively little risk. Although these procedures may not cause a visible short-term cosmetic problem, they unnecessarily destroy precious donor hair and limit the amount of fullness that can ultimately be achieved. Even procedures touted as state-of-the-art technology, such as “laser hair transplantation,” can cause harm to the unwary patient ((Bernstein RM, Rassman WR. Laser hair transplantation: Is it really state of the art? Lasers in Surgery and Medicine 1996; 19:233-235.)) by slowing the healing process and causing unnecessary scarring.
A number of excellent publications have been written on the subject of repair. ((Lucas MW. Partial retransplantation. A new approach in hair transplantation. J Dermatol Surg Oncol 1994; 20:511-4.)), ((Brandy DA. Techniques for the refinement of abrupt hairlines and donor scars secondary to obsolete punch hair-grafting and flaps. Am J Cosmet Surg 1995; 12:341-4.)), ((Unger WP. Correction of Poor Transplanting. In: Unger WP, ed. Hair Transplantation, 3nd ed. New York: Marcel Dekker, 1995:375-388.)), ((Leavitt ML. Corrective hair restoration. In: Stough DB, Haber RS, eds. Hair Replacement: Surgical and Medical. St. Louis: Mosby Year Book, Inc., 1996:306-314.)), ((Swinehart JM. Hair repair surgery. Corrective measures for improvement of older large-graft procedures and scalp scars. Dermatol Surg 1999; 25(7):524-529.)), ((Vogel JF. Correcting frequently seen hair transplant problems. Hair Transplant Forum Intl. 2001; 11(1): 5-8.)) The goal of this paper is to present further insights into repair strategies and expand upon the techniques that are needed to implement these restorative procedures successfully. It is our intent that this article serve as a practical guide for physicians attempting to repair the problems they encounter in their daily practices and enable those surgeons performing hair restoration to identify some common pitfalls in advance – so that these problems may ultimately be prevented.
The Problems
The major cosmetic problems encountered with poorly planned or improperly executed, hair restoration surgery can be classified into the following interrelated categories:
• Grafts that are too large or “pluggy”
• A frontal hairline placed too far forward
• A hairline that is too broad
• Hair placed in the wrong direction
• Areas of attempted coverage that are unrealistic
• Scarring in the recipient area
• Ridging
• Donor scarring
• Low or depleted donor supply
Large or “Pluggy” Grafts
It is unfortunate that in the United States, hair restoration got off to a start in the wrong direction. In this country, the use of large 4mm grafts began in the late 1950s. In Japan, a more delicate procedure, using 1- to 3-hair micrografts, had been performed since the early 1940s. ((Stough DB. The origins of single-hair grafting. In: Stough DB, Haber RS. Hair Replacement: Surgical and Medical. St. Louis: Mosby-Year Book, Inc., 1996:187.)) If the West had been aware of this technology sooner, countless patients could have been spared cosmetically disfiguring surgery. It took American physicians until the early 1980s to realize that using small mini- and micro-grafts would produce superior cosmetic results ((Marritt E. Single-hair transplantation for hairline refinement: a practical solution. J Derm Surg Oncol 1084; 10:962-966.)) and another 10 years before their use became widespread.
There are multiple problems with transplanting larger grafts. When hair is distributed properly in a hair restoration procedure, the density should not exceed 50% of the patient’s original density. The reason for this is that the normal human scalp has at least a 100% visual redundancy. This means that the eye cannot perceive hair loss until it exceeds 50%. ((Marritt E. The death of the density debate. Dermatol Surg 1999; 25:654-660.)) Due to this redundancy, there is no reason to restore more than 50% of the hair, especially in view of the fact that the balding individual has less total hair volume. The density of hair in plugs, however, actually exceeds the donor density due to elastic contraction of grafts, unless there is significant hair wastage from the grafting itself.
The high density of large grafts produces a pattern of excessive hair within the grafts and empty spaces between them. In most patients who will have a significant amount of balding, there is not enough donor hair to both fill in the spaces between the plugs and cover the entire area that needs hair. As a result, the surgeon is left with the dilemma of choosing between a pluggy look scattered over a large area, or very high density in some areas with insufficient coverage in others – neither a desirable option for the patient

In clinical practice, one often observes less density in the grafts than anticipated from the size of the harvested plug. This can be due to a number of different factors. Two of the most common are loss of hair from poor harvesting techniques and hair loss caused by a phenomenon called “dough-nutting.” In dough-nutting, the centers of grafts receive insufficient oxygen following transplantation and, therefore, the follicles in the central portion of the grafts fail to survive. This results in hair growth limited to the periphery of the grafts. Dough-nutting was a phenomenon seen with 4- and 5-mm plugs, but also with grafts 3-mm in size. Although more common with poorly executed large graft procedures, it does not occur with micro-grafts or follicular unit grafts. A “crescent” deformity occurs when the pattern caused by transection is superimposed upon the pattern caused by central hypoxia. The transection, in effect, cuts off half of the doughnut leaving a crescent shape.


Hairline Too Low or Too Broad
Although the adolescent hairline hugs the upper border of the frontalis muscle, the position of the normal adult male hairline is approximately one fingerbreadth higher (1.5cm above the upper brow crease at the midline).4 A common mistake of the inexperienced hair restoration surgeon is to restore the hairline to the adolescent, rather than the normal adult location. This mistake is frequently made on younger patients whose memory of their adolescent hairline is still fresh in their minds and who put considerable pressure on the doctor to place hair in this location. Unfortunately, it also occurs in situations where the physician is anxious to get the patient “started” with surgery rather than initiating a more conservative (and more appropriate) medical treatment. A low frontal hairline not only distorts the patient’s facial proportions, it sets expectations that are unsustainable if the balding progresses, and precludes a natural, balanced look to the restoration as the patient ages.3
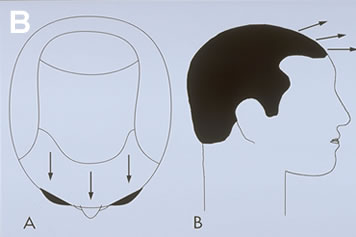
The patient whose hairline has been placed too low often has a hairline that is also too broad. The low-broad hairline is far more unnatural and far more difficult to correct than correctly positioned plugs. A variation of the low-broad hairline is the “two-horned hairline.” This results when a doctor fills in the corners of a Norwood Class 2 or Early Class 3 balding pattern and then the person proceeds to lose the central, non-transplanted portion of his scalp, isolating the transplanted sides and leaving two horn-like hair patches (Figure 8A).
Hair Placed in the Wrong Direction
In the front and top part of the scalp, hair grows in a distinctly forward direction, changing to a radial pattern as it approaches the crown. The hair always emerges from the scalp at an acute angle, with the angle being most acute at the temples. In order for the transplant to look natural, the patient’s own hair direction must be closely followed. The one exception is that whorls, or licks, at the frontal hairline should not be duplicated if there is a good chance that the area will be lost because of balding. In this case, it is better to transplant the hair in the more neutral position, characteristic of the majority of men.

There has been a tendency for hair restoration surgeons to transplant larger grafts perpendicular to the skin. This is probably because the mechanics of the old plug procedures made sharp angling technically difficult and, if angled, resulted in more elevation and/or pitting when the grafts healed. Grafts often become slightly more perpendicular to the skin, compared to the way they were originally placed, as a result of the normal healing process. This perpendicular movement tends to magnify any errors in the transplant and is a phenomenon seen with grafts of all sizes. It is probably caused by the reorganization of collagen around the newly transplanted grafts.
The consequence of placing grafts perpendicular to the skin is most apparent when this mistake is made in the frontal hairline. A “Statue of Liberty” appearance results when the transplanted frontal area has hair pointing in radial directions. This makes combing the hair in any style problematic and invariably results in an unhappy patient.
Another problem with placing hair perpendicular to the scalp is that the viewer looks directly at the base of the hair shaft (i.e. where the hair inserts into the scalp). This contrasts with normal hair growth, or with a properly performed hair transplant, where the hair points forward. When hair planted in a forward direction is groomed, the hair shaft bows presenting the convexity of the hair shaft to viewer. This makes the hair appear more soft and natural and gives a subtle fullness to the transplant.
Unrealistic Area of Coverage
Attempting to cover an area greater than the donor supply can adequately fill may leave cosmetically important areas thin or not transplanted at all (Figure 4). It is important to remember: The first region to bald is the area where you should be most hesitant to transplant. For example, the temples and crown generally bald first, but recession at the temples and thinning in the crown are very acceptable, especially as the patient ages, and these areas may be left untransplanted. The central forelock region, however, is generally late to bald (particularly in certain family lines), but when it is lost the patient loses the frame to his face and its restoration becomes essential. This useful guideline is commonly ignored by doctors in a hurry to start surgery on their patients.

An adequate amount of hair must always be reserved for critical areas, such as the forelock and top of the scalp, regardless of whether these areas need coverage at the time of the initial transplant. If the patient’s donor reserves are limited due to poor scalp laxity, low donor density, fine hair shaft diameter or a host of other reasons, the transplantation of other, less critical areas should be postponed or avoided all together. A pattern that resembles “two horns and a tail” may result when surgeons are too aggressive in transplanting the temples and crown in a young person. As the name suggests, this seemingly benign procedure becomes a cosmetic nightmare for the patient when there is further balding and these regions cannot be connected due to inadequate donor reserves.
Scarring in the Recipient Area
In surgical procedures, the general maxim applies the greater the wound, the greater the scar. Hair transplantation is no exception. Traditional round grafts result in the largest wounds, but even mini-micrografting produces wounds that can be unnecessarily large since, in this technique, most of the donor tissue is transplanted along with the hair.5
Scarring has a number of undesirable effects on the transplant. It decreases the resiliency of the connective tissue and alters blood flow. It can distort hair direction and cause a change in the quality of the hair shaft itself. When severe, scarring can cause graft elevation or depression, loss of grafts post-operatively and poor hair growth. When mild, it may result in subtle textural and visual irregularities in the skin. All of these factors serve to decrease the chance of a cosmetically satisfactory result.
It has been the experience of these authors that, to achieve optimal cosmetic results, the upper limit of recipient wound size should be no more than a 1.7mm slit (the approximate size made by an 18 gauge Nokor needle). At 1.7mm, or less, there is little chance of any surface change from the wounds/grafts. At wound sizes greater than this, the incidence of surface change increases significantly. Since it is very difficult to determine in advance which patients will be affected, it is preferable to keep recipient wounds at or below this limit.
Laser hair transplantation, more aptly termed “laser site creation” represents the epitome of purposeless scarring.8 The laser used in this context represents nothing more than a marketing gimmick to re-package the old punch technique as a “state-of the art” technology. The laser is a glorified “punch” that creates holes or slits in the recipient scalp by removing (vaporizing) tissue. The laser is smartly marketed with claims that “the beam is so precise that the zone of thermal injury can be measured in microns.” However, regardless of how little damage is done to surrounding tissue, the recipient tissue directly under the beam is destroyed.
The laser may offer the short-term advantage of less bleeding and faster site creation, but has the significant disadvantages of increased set-up time, greater cost and potential eye hazards. Most important, the laser destroys scalp tissue and unnecessarily increases recipient wounding.
Ridging
Another cosmetic problem that may be caused by using larger grafts is the extra volume of tissue introduced into the recipient site. This extra tissue can produce a fullness and elevation of the transplanted area that results in a ridge of skin, demarcating it from the surrounding bald scalp.2 In some patients, this problem is compounded by a proliferative reaction of the surrounding tissue in response to the transplanted grafts or, according to Dr. Martin Unger, a foreign body reaction to hair spicules and other debris trapped at the time of surgery. This phenomenon, termed “hyperfibrotic healing” by Unger, ((Unger M. Hyperfibrotic transplants. Hair Transplant Forum 1993; 3(4):8-9.)) accentuates the abnormal contour of the transplanted area. In addition, there is some evidence that the hair subsequently placed into this area may exhibit suboptimal growth.
Whereas contour change due to excess volume is directly related to the size of the transplanted grafts, hyperfibrotic reactions appear to be more idiosyncratic and related to the underlying genetic predisposition of the individual. In spite of this, hyperfibrotic changes are rarely seen with very small grafts and have not been reported with Follicular Unit Transplantation.
Donor Scarring
Although the major impact of scarring in the donor area is to decrease the amount of available hair for future hair transplants, when severe, the scar itself may be a cosmetic problem. This is most likely to occur when the scar is: 1) placed too high (in the non-permanent zone), 2) placed too low (near the nape of the neck or over the ear), 3) excessively wide in any location, 4) hypertrophic or keloidal, or 5) a result of extensive open donor harvesting. This important subject will be covered in more detail in the section Donor Repair.
Low or Depleted Donor Supply
A low or depleted donor supply is usually the least obvious of the cosmetic problems encountered with poor hair restoration surgery, but is the major limitation to achieving adequate density or sufficient coverage in future procedures. It is the “hidden enemy” of repairs (Figure 5).

A low or depleted donor supply results from wasting hair during the surgery. Hair wastage has many causes: poor graft harvesting and dissection, poor donor closure, improper graft storage and handling, transplanting the grafts too close together, using grafts that are too large, creating wounds that are too big, poor pre-operative preparation, and inadequate post-operative care. Every step of a poorly executed transplant may contribute to depleting the patient’s donor supply.
An interesting paradox occurs with the old punch-graft technique. When the procedure is executed flawlessly, most of the donor hair is captured in each punch and the growth of the grafts can appear pluggy. When the procedure is performed poorly, there is increased transection of the harvested follicles and inadequate growth in the centers of the larger grafts, creating a somewhat softer, more natural look (see previous section on “Large Grafts”). Although in the latter situation patients may be satisfied initially, the poor growth can cause problems in hair supply down the line and ultimately a worse cosmetic result.
The Limitations
Many of the cosmetic defects created by poor techniques can be partially or completely reversed by meticulously removing and re-implanting unsightly grafts. However, the main factor that generally prevents the surgeon from achieving all of the patient’s restoration goals is a limited donor supply.
Hair wastage due to poor surgical techniques, as discussed above, is usually the main cause of donor supply depletion. The early telltale signs of hair wastage may be a transplant that appears too thin for the number of grafts used, poor growth manifested as gaps at the hairline, or uneven density in areas where the coverage should be uniform. The fact that donor hair was wasted might be surmised from a donor incision that was longer than expected for a given number of grafts, or an abnormally low density in the donor area near the donor scar. Unfortunately, it is very difficult to ascertain the exact underlying causes after the fact and, by the time surgeon is aware that he has run out of usable donor hair, the damage to the patient has been done.
Because an adequate donor supply is so critical to a successful repair, accurately assessing the amount of hair available becomes paramount. When performing a hair transplant procedure on a virgin scalp, quantifying the donor supply is rather straightforward, as density and scalp laxity are relatively uniform in the donor area. In repairs, however, additional factors come into play. Even though there may appear to be enough hair in the donor area, it may not be surgically accessible. Factors that limit the available donor hair include:
• Low donor density
• Fine hair caliber
• Poor scalp mobility
• Scarring
Low Donor Density
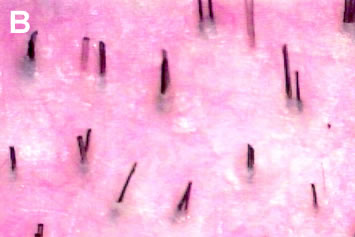
Donor hair density (donor density) can be measured using a simple hand-held device called a Densitometer. ((Rassman WR, Pomerantz, MA. The art and science of minigrafting. Int J Aesthet Rest Surg 1993; 1:27-36.)) This instrument is invaluable for the assessment of donor density, follicular unit composition, and miniaturization. The average Caucasian has approximately 2.1-2.3 hairs/mm2, but this can vary from as little as 1.5 hairs/mm2, to greater than 3 hairs/mm2.4,5 In most individuals, the density of follicular units in the scalp is relatively constant at 1 follicular unit/mm2 (Figures 6A, B). Thus, patients with high hair density have more hairs per follicular unit, rather than having follicular units spaced more closely together. The converse is also true. A person with naturally low hair density would have fewer hairs per follicular unit, but with the same spacing between the units (i.e., 1 follicular unit/mm2). At very low densities, this rule is less applicable.

The scarring produced by the traditional punch-graft method, that used the open-donor technique to harvest the hair, is a visible marker of the amount of surgery performed.5 One can easily estimate the amount of donor hair used by comparing the area of open-donor scarring to the remaining virgin donor scalp. In strip-harvesting, however, the linear scar gives little indication of the strip’s original size, since it only reflects the length of the excised skin and not the width. With this method, the actual amount of tissue removed cannot be easily ascertained.
Using densitometry, one can deduce information regarding a previously excised donor strip, albeit indirectly. When a donor strip is removed and the edges sutured together, the surrounding skin is stretched, increasing the space between naturally occurring follicular units. The number of hairs per follicular unit, however, will remain unchanged and will reflect the patient’s original donor density. For example, if the patient had a donor density of 2.4 hairs/cm2, he would have a follicular unit density of 1 follicular unit/cm2 (as discussed above) and average 2.4 hairs per follicular unit. After the procedure, his average hair density might drop to 2.1 hairs/cm2, but the follicular units in his donor area would still contain an average of 2.4 hairs each. The spacing between follicular units, however, will increase due to the surgery, and so now his follicular unit density would measure 0.875 follicular units/mm2, instead of the normal 1/mm2, representing a 12½% decrease.
The percent decrease in follicular unit density will provide an indication of how much tissue was removed and more important, how much remains to harvest. In general, a person’s follicular unit density can be decreased to approximately 0.5 units/cm2, before the donor area will become too thin and no more hair should be harvested. Therefore, if the follicular unit density in the area of previous donor harvests measures 0.75/mm2, approximately half of the potential donor hair has been used and approximately half of the usable hair remains. In the example given above, a 12.5% decrease in follicular unit density means that 25% of the available donor hair in that area was used in the prior procedure.
The value in measuring both follicular unit size (hairs/follicular unit) and follicular unit density (follicular units/mm2) is that the former gives the surgeon information about the patient’s original hair density, and the latter about how much hair has been used in previous surgeries, even when the patient’s original hair density had not been measured.
Fine Hair Caliber
Although not affected by the transplant, hair shaft diameter is an extremely important contributor to hair volume and thus available hair supply. Hair shaft diameter is less often mentioned than the actual number of hairs because it is more difficult to measure. However, its importance in both the virgin transplant and in a repair procedure cannot be overemphasized.
The range in terminal hair shaft diameter is approximately 2.3 fold (0.06 mm for very fine Caucasian hair to 0.14 mm for coarse Asian hair). ((Bernstein RM. Measurements in hair restoration. Hair Transplant Forum Intl. 1998; 8(1):27.)) This represents a variation in x-sectional area of approximately 5.4 fold, since area = ~r2 or ~(1/2d)2. In contrast, the range in hair density in patients that we transplant is from 150 hairs/cm2 in those of low density, to approximately 300 hairs/cm2 for those with the highest, a 2-fold difference. If we compare this to the 5.4 fold range in hair cross-sectional area, we see that, in theory, variations in hair shaft diameter should have a 2.7 times greater impact on the appearance of fullness (visual density) than the absolute number of hairs (Figures 6A, B).
The importance of this in a repair is that, for a given degree of plugginess, fine hair will provide less camouflage than coarser hair. Therefore, fine hair must be transplanted in greater numbers or in multiple sessions to achieve the same degree of camouflage. When this quantity of hair is not available, compromises must be made in the repair.
Poor Scalp Mobility
Donor density and hair shaft diameter are not the only factors affecting the available donor supply. In order for an adequate amount of hair to be harvested by the strip method, there must be sufficient scalp laxity to close the wound after the donor strip is removed. In the face of a low donor density, having adequate scalp laxity is especially important because a widened scar may be visible through the thin hair.
The location of the donor incision greatly affects scalp mobility. The ideal position for the donor incision is in the mid-portion of the permanent zone that lies, in most individuals, at the level of the external occipital protuberance and the superior nuchal line. The muscles of the neck insert into the inferior portion of this ridge, so that an incision placed below this anatomic landmark will be impacted by the muscle movement directly beneath it. A stretched scar in this location is extremely difficult to repair since re-excision, even with undermining and layered closure tends to heal with an even wider scar. To compound the problem, one is more likely to cut through fascia with a low donor incision; once the fascia has been violated, the risk of having a widened scar is greatly increased.
Incisions placed significantly above the occipital protuberance have a greater incidence of widened scars, but this risk is not as great as it is when incisions are placed below the occipital protuberance. The main risks of placing scars too high on the posterior scalp are lack of permanence of the transplanted hair (it may be subject to androgenic alopecia) and future visibility of the scar if the donor fringe were to narrow further.
In “Follicular Unit Extraction,” a technique using very small punches (~1mm) to remove individual follicular units directly from the donor area without using a linear incision, the problem of a tight scalp may be circumvented. This procedure is somewhat analogous to the old punch technique except that, in addition to merely keeping the punches aligned parallel to the hair shafts, the punches are now fitted over individual follicular units. When using this procedure for repairs, follicular transection can be a significant problem, because the alignment of the follicles is often distorted by scar tissue.
Scarring
Scarring in the donor area limits the amount of hair accessible to the surgeon for a number of reasons. The most obvious is that a larger donor strip must be removed to harvest the same amount of hair. The second, mentioned above, is that scarring decreases scalp laxity by destroying elastic tissue and obliterating the subcutaneous space. This causes the dermis to be bound down to the fascia below. The third is that the scars themselves may be visible and require more hair to be left in the donor area to cover the scarred area than would be necessary to cover normal scalp.
With the objective of avoiding transection, but in the face of poor visualization, the surgeon using the traditional punch technique often passed completely through the sub-cutaneous space to ensure that he was below the level of the hair follicle. Because many individual punches were needed, this could result in significantly more obliteration of the sub-cutaneous space than produced by a linear incision. The very nature of secondary intention healing, on which the open donor technique depended, caused a significant amount of scarring in the donor area.
The presence of open donor scars may give the surgeon a false sense of security thinking that, because an excision with a primary closure was not performed, the patient’s donor laxity has not been compromised. This logic may lure the unwary surgeon into harvesting a donor strip that is too wide, often with disastrous consequences. When the surgeon attempts to close the donor wound, the tight closure requires more tension on the sutures. The sutures, however, tend to tear the scarred wound edges, since scar tissue is significantly less elastic and more friable than normal scalp. An attempt to redistribute the tension by undermining runs the risk of causing additional trauma to a greater area and may result in an even larger wound.
Basic Repair Strategies
Establishing Priorities
Before repairing an old transplant, it is important to establish what aspects of the prior surgery are most bothersome to the patient. One should not assume that what concerns the cosmetic surgeon would also be a problem for the patient. It is important to have the patient prioritize his concerns and to discuss the management of each concern with him. It may not always be possible to resolve all of the patient’s concerns, but limited improvement may still be a worthy goal. Some aspects of the transplant that bother the surgeon may be left untreated if they do not concern the patient. Establishing a hierarchy of priorities before the repair is started will ensure maximum patient satisfaction.
A hierarchy of complaints might be:
1. “My crown is bald”
2. “My hairline is too pluggy”
3. “My hairline is too high”
The pluggy hairline may be improved by punching out and re-distributing some of the hair in the large grafts. This would be particularly convenient to solve since an additional concern is that the patient’s hairline is too high. Camouflage can be accomplished by placing a transition zone of follicular units in front of the larger grafts. This would require very little additional hair. On the other hand, the complaint of a bald crown may not be treatable if the patient’s donor reserves were severely depleted from the prior procedures. Before the repair is started, it is important for the surgeon to explain to the patient which goals are actually attainable, so that the patient may set his expectations appropriately.
It is also important to identify the underlying cause of the patient’s complaint. For example, if a patient complains that his hair is not groomable, it may be that scarring around the grafts has caused the hair to grow in a kinky or wiry fashion. This situation can only be improved by planting smaller grafts in normal skin in front of the wiry hair. On the other hand, if the difficulty in grooming had been caused by hair placed in the wrong direction, the improperly placed hair would have to been removed and re-implanted correctly.
Examples of some common complaints and their causes are listed Table 1.
Formulating a Plan
Two basic repair strategies that are often used in conjunction with one another are: 1) camouflage with follicular unit grafts and 2) removal of grafts with re-implantation of hair as individual follicular units. Unless otherwise specified, when we use the term camouflage we will be referring to the procedure where donor hair is taken from the donor area in the back or sides of the scalp and transplanted into the recipient area with the intent of improving the appearance of previous work. The term re-implantation is used when the donor hair is derived from the microscopic dissection of excised grafts or plugs. “Re-implanted hair” can of course, be used for camouflage as well, but since graft removal most often takes place at the frontal hairline, the hair that is derived from these grafts is usually placed slightly further back, away from the hairline.
Camouflage
Camouflage is the primary means of improving the appearance of a poorly executed transplant. Existing grafts are used to provide volume or bulk to the transplant and the camouflage, created by follicular units or small mini-micrografts, is used to create a more natural appearance. When possible, camouflage should be used as the sole restorative procedure, as excision and re-implantation require additional procedures and will postpone the completion of the restoration. In addition, the process of removing grafts may cause some damage to the hair follicles and produce additional scarring. Since removal of large numbers of grafts may result in less total hair volume, grafts should not be removed indiscriminately. However, it has been our overwhelming experience that, if there is any question about whether specific grafts should be removed, it is in the patient’s long-term best interest to err on the side of removal, rather than on camouflage alone.
Creating camouflage by building a transition zone in front of existing grafts, rather than attempting to fill in the area between the grafts, has two important advantages. First, it generally produces the maximum cosmetic benefit using the fewest number of grafts. Second, it often allows the surgeon to place hair in normal skin, rather than in an area of scarring where growth may be inconsistent (Figures 7A, B). Particularly when donor reserves are limited, creating camouflage around the periphery of a problem area and then using a specific grooming technique to enhance the appearance of the transplant is the most efficient way of using small amounts of donor hair (Figures 8A, B).




Removal and Re-implantation
Camouflage should be preceded by excision and re-implantation of individual follicular units when camouflage alone is incapable of producing satisfactory results. This situation usually occurs when:
• Grafts are too large to be camouflaged
• Grafts are in an inappropriate location
– The hairline is too low or too broad
– The temples have been inappropriately transplanted
– The crown has been transplanted in a person with an inadequate donor supply
• The hair direction is wrong
• The density of a transplanted area is so great that it cannot be balanced by simply adding hair to other areas of the scalp
When grafts are too large and located in a position where placing additional grafts in front of them would bring the hairline down too low, when the hair that the grafts contain is pointing in the wrong direction, or when the grafts are located in an area that should not have been transplanted, their removal is mandatory. Camouflage alone in these situations will likely exaggerate an already unacceptable appearance. When the density of hair in the transplanted area is too great, excision and re-implantation can re-distribute the hair over a larger area. When large grafts were transplanted in the forelock area, camouflage alone is often successful. However, when large grafts were used to create a dense frontal rim, aggressive re-implantation is almost always required.
It is important to stress that the best results are achieved when excision and re-implantation are performed before camouflage is undertaken. Once additional grafts have been placed, removing the old ones becomes much more problematic and additional hair wastage and scarring can result. If there is any doubt that an existing graft can be adequately camouflaged, it is best to err on the side of removing all, or part of the graft, rather than relying on camouflage alone (Figures 9A-C).



A common approach to improving the appearance of plugs is to attempt to fill in the empty spaces between the grafts with additional large grafts. The main problem with this method, however, is that it takes an area of already high density and makes it even greater. Since the resulting density is often impossible to sustain, the patient runs a serious risk of completely depleting his donor reserves. This, in turn, may force the surgeon to leave gaps in the area being repaired, and leave other cosmetically important areas uncovered. Another problem is that the use of large grafts in the repair produces additional scarring and decreases blood supply in an area that is already markedly scarred from prior procedures. As a result, the new grafts may exhibit poor growth, and there is a decreased chance of future procedures being successful.
An approach preferred by these authors for improving the appearance of plugs, is to reduce the density of these larger grafts by excising a portion of them and then redistributing the hair from these grafts into an adjacent area as individual follicular units. This will decrease the density of the problem area and permit additional areas to be transplanted with less density, since potential contrast will have been reduced. This, in turn will produce a more balanced look and conserve donor hair in the process.




