Robert M. Bernstein, MD, New York, NY
Hair Transplant Forum International 1998; 8(3): 23-25.
The introduction of the “Follicular Family Unit” by Dr. David Seager ((Seager D. Dense hair transplantation from sparse donor area – introducing the “follicular family unit.” Hair Transplant Forum International, Vol. 8, No. 1:21-22, 1998.)) (Forum Vol. 8, No.1, 1998) is a welcome expansion of the technique of follicular unit transplantation. The focus of this discussion is to highlight areas in which, in my opinion, the “follicular family unit” can add to the power of follicular unit transplantation, but also to caution about areas in which its use might actually detract from the ability to produce the most natural results. The density of follicular units in the human scalp is approximately 1 unit/mm. ((Bernstein RM, Rassman WR, Szaniawski W, Halperin A: Follicular transplantation. International Journal of Aesthetic and Restorative Surgery 3:119-132 1995)) This is an average, however, and the spacing between individual units can vary considerably. In addition, follicular units are closely grouped in the mid- and upper dermis (figure 1), but at their deepest portion (in the upper sub-cutaneous fat); their distribution is practically random (figure 2). As a result, the individual follicles within each unit will have changing relationships to one another as they course through different levels of the skin. Both of these factors contribute to the complexity of the dissection and, as a result, the dissector must make continuous “judgements” of inclusion and exclusion. The importance is that the close proximity of the follicles allows for a compact implant that can fit into a small recipient site.2
If the “follicular family unit” truly represents only the inclusion of stray hairs that might belong together naturally, due to their close proximity to the nuclear family, then one could hardly argue that these should not be included. If one adheres to Dr. Seager’s recommendation that “One must find two separate units that look close enough to almost belong together…” or “dissecting closely contiguous one-and two-haired units together,” then site sizes should not need to increase to any substantial degree, and the technique should be valuable. In fact, it might always be better to include these “strays” as they might be subject to fewer traumas than if they were dissected away.
On the other hand, if including extended members of the follicular family requires a larger house (i.e. a larger site) then the recipient wounding will be increased, the hair/skin ratio of the graft will not be maximized, and the benefits of follicular unit transplantation will be diminished.2 In general, a shift from a 19 gauge to an 18 gauge needle for site creation, is not very significant, especially behind the frontal hairline. However, a shift from an 18g to a 16g needle site to accommodate concomitantly larger grafts, in my opinion, can present problems, as this size site can on occasion lead to surface changes and an unevenness in distribution that is never encountered with pure follicular unit transplantation.2 In addition, the altered scalp makes subsequent procedures more problematic.
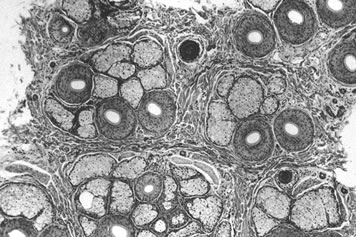 Figure 1. Transverse microscopic anatomy of the normal adult male scalp at the level of the sebaceous glands shows groupings into distinct follicular units.
Figure 1. Transverse microscopic anatomy of the normal adult male scalp at the level of the sebaceous glands shows groupings into distinct follicular units.Of the examples given, using slightly larger grafts to correct “bad hairlines created with compressed minigrafts or old plugs” is the most problematic. Often these patients not only present with a “pluggy look” that can be corrected by adding hair, but also with volume changes due to the excess skin moved. This, in combination with the “hyperfibrotic” changes that they may elicit (I find this to be much more common finding than originally described ((Unger MG: Hyperfibrotic transplants. Hair Transplant Forum International, Vol. 3, No. 4:8-9 1998.))), can alter the overall contour of the patient’s scalp and present additional problems in the repair. In these instances, even the slightest increase in additional skin volume may worsen, rather than improve, the patient’s appearance. It is certainly helpful to use 3- and 4-hair follicular units in front of old plugs for better camouflage, if they occur naturally, but I would argue that in this situation, rather than combining units with their concomitant increase in tissue bulk, it would be better to accomplish the goals in a second session. This is especially true where the pluggy hairline is already in a forward (low) position and the zone of camouflage cannot be made too deep.
The second situation of concern, is the female hairline. The female hairline is always the most delicate, and is naturally composed of fine, vellus hairs at the leading edge ((Bernstein RM, Rassman WR: The aesthetics of follicular transplantation. Derm Surg 1997;23:785-799.)). I would be hesitant to grafts larger than compact follicular units in the hairline or even “the part” as, in these locations, even the slightest surface irregularity or unevenness in distribution will be detected as the patient continues to thin. More importantly, I would question the wisdom of transplanting a woman with “diffusely thinning hair loss over the entire scalp including the donor area” as the donor hair in these patients is, by definition, not permanent and will continue to be lost after it is transplanted. In addition, these women with “diffuse unpatterned alopecia” ((Bernstein RM, Rassman WR: Follicular transplantation: patient evaluation and surgical planning. Derm Surg 1997;23:771-784.)) often become extensively bald and the even small grafts tend to become isolated over time. In the case of women with diffuse hair loss, but a stable permanent zone (diffuse patterned alopecia) transplantation is occasionally warranted to re-create a hairline that can be used to soften the edge of a hairpiece or to camouflage a larger area of thinning behind it. However, in both of these situations, the patient often desires to wear her hair pulled back so the detail of the frontal hairline is visible and must be must be exacting. In both of these situations, multiple procedure are generally needed and in my experience the goal of recreating a satisfactory female hairline can rarely be accomplished in one session.
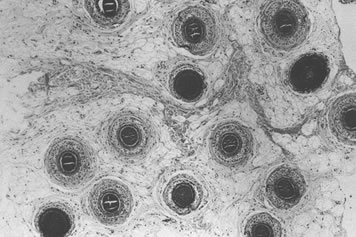 Figure 2. Scalp shown in a horizontal plane at the level of the upper sub-cutaneous fat showing a random distribution of follicles.
Figure 2. Scalp shown in a horizontal plane at the level of the upper sub-cutaneous fat showing a random distribution of follicles.In the third situation (the patient with very fine, light colored hair), it is stated that “Four sessions of successful 4-mm punch grafts that produce complete growth will not provide sufficient density in these areas because the donor area is simply not dense enough.” It is then offered that “creating three- or four-haired follicular units out of suitably adjacent smaller units offers a totally new method for achieving an extremely natural looking transplant with increased density using sparse donor area.” This is the most puzzling comment of all. The article begins with “The ultimate, maximum density of a hair transplant is limited by fixed, unchangeable factors, such as donor hair density, color and texture, and hair shaft diameter.” If this statement is correct, then how can one increase the density of the transplant beyond that of the thin donor area (especially if only one session is used)? This logic seems to revert to a “pre-modern” period of thinking in hair restoration when it was felt that a patient could be transplanted with larger grafts that, when packed wall to wall, would create an ideal density, no gaps, cover the entire bald scalp, and never have the patient’s donor supply run out. I would offer that a patient with fine, light colored donor hair of low density should have a fine, light transplant, as a final result.
The last example, “building up the anterior temporal fringes in the extensively bald patient” also seems problematic for follicular family units. The most difficult aspect of reconstructing the temple hairline is creating angles so acute that the emerging hair lies flat against the skin surface. When grafts larger than very compact one- and two-hair follicular units are used, I have found it much more difficult to achieve this effect. In addition, any increased bulk to the graft can produce an irregularity in the very fine temporal skin. It is then stated that “It is otherwise very difficult to achieve a natural looking high density in these prominent and conspicuous areas without multiple micrografting sessions.” I wonder whether one would want to achieve high density in the “anterior temporal fringe of an extensively bald patient” and if one were, I would think that several sessions using the most delicate of grafts would be the best way to approach the problem.
One never wants to subject the patient to a protracted course of multiple surgeries5, but in aesthetically “delicate” areas such as repair work, hairline reconstruction, temple restoration, and the treatment of women, trying to achieve all of one’s goals in a single session may not be possible, even when recruiting more family members for help. It would seem that the “follicular family unit” can be useful in situations where the strict “definition” of the naturally occurring follicular unit could be slightly broadened without compromising the aesthetic outcome of the transplant. However, in the examples above, I feel the more compact, naturally occurring, individual follicular unit would be the best choice.
In summary, it seems that some of these new additions may be old family members dressed up in new clothes, and we are, of course, happy to have them around. We should remind ourselves that since family reunions may be held more than once, we don’t necessarily need to accomplish everything in one visit. I would readily welcome new members of the “follicular family unit” as long as they were reasonably compact, and could be placed into very small recipient sites. However, if the new members were of a size that necessitated a move into a larger home, then I would be cautious about having them in our neighborhood.




