Minimizing the scar from the donor incision is a critical part of a successful hair transplant procedure. A fine donor scar allows a person to keep his/her hair relatively short after the hair restoration (if one wants to do so) and increases the amount of hair that can be harvested (removed) in subsequent hair transplant procedures.
A number of techniques have been developed to minimize donor scarring when using a strip excision during FUT Hair Transplant surgery. These include the use of tumescent anesthesia, undermining, absorbable sutures, buried sutures, staples and trichophytic closures. The technique of FUE Hair Transplant surgery, where follicular units are removed directly from the scalp without a linear incision, is covered in another section.
Strip incisions are widely used because they enable the hair transplant surgeon to efficiently perform large hair transplant sessions, while at the same time, minimize damage to hair follicles. The reason this is possible is because the strip of donor tissue that is removed from the scalp is placed under a series of stereomicroscopes where the individual follicular units can be dissected from the tissue under direct visualization (see Graft Dissection).
There are four main aspects to having the donor incision heal in a fine line; 1) placing the incision in the proper location 2) using the correct donor strip dimensions, 3) removing the strip without damage to the tissue, and 4) closing the donor area with impeccable surgical techniques.
Position of the Donor Incision
The ideal placement of the donor incision is in the mid-part of the permanent zone located in the back and sides of the scalp. This area lies in a band that starts above the occipital protuberance (the bump felt in the middle part of the back of the scalp) and extends to either side in a gentle, upward sloping curve that follows the contour of the scalp. If hair is harvested below this region, there is a greater risk of scarring from the wound stretching, since the incision will be too close to the muscles of the neck. If the incision is above this area, the hair may not be permanent and may fall out as the baldness progresses.
Size of the Donor Strip
Although the length of the donor incision is determined predominantly by the number of follicular unit grafts required for the hair restoration, the width (height) of the donor incision depends upon the patient’s scalp laxity. This is a genetic attribute of the patient’s scalp that must be carefully measured by the hair transplant surgeon during the initial evaluation. With good scalp laxity, a wider strip may be harvested from the donor area without the risk of scarring (although patients with very loose scalps may be at increased risk of a wide scar (see Dr. Bernstein’s publication, “Scalp Laxity Paradox“). If the scalp is too tight, taking a normal size strip may be impossible.
If the strip width is too narrow, the incision will need to be unnecessarily long to obtain an adequate amount of donor hair. If the strip width is too wide, the risk of having a widened scar will be increased significantly. Expert clinical judgment, acquired over years of experience, is needed for the surgeon to consistently set the appropriate length and width of the donor strip and achieve the minimum possible scar.
Most patients have 90-100 follicular units per cm2 in their donor area. Therefore, in a hair transplant of 2,000 follicular unit grafts, a donor strip that was 1cm wide would need to be slightly over 20 cm long to yield the appropriate number of grafts.
Scalp Laxity Exercises
- Scalp Exercises
- Download Instructions
In Follicular Unit Transplantation your physician will obtain donor hair from a long, thin strip removed from the back and/or sides of your scalp. The procedure can most easily be accomplished when the scalp is moderately loose as it enables the surgeon to harvest more grafts. A tight scalp can be loosened using the following simple exercise.
- Place the palm of your hands on the back/sides of your head with your fingers pointing upwards and thumbs pointing towards each other.
- Move the scalp up and down as vigorous as possible using your palms and thumbs, with the fingers resting stationary on the top of your scalp.
- To stretch the entire donor area, use three different positions for the palm and thumbs:
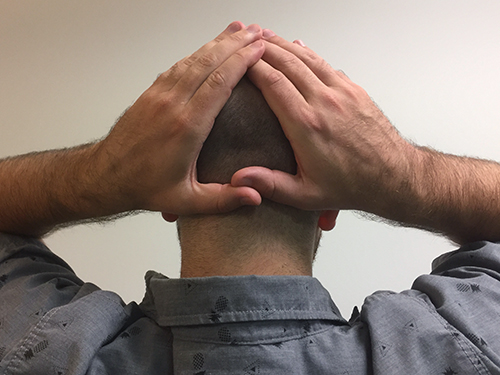 1. Palms in back of scalp with thumbs overlapping
1. Palms in back of scalp with thumbs overlapping 2. Palms on sides of scalp with thumbs touching in the back
2. Palms on sides of scalp with thumbs touching in the back 3. Palms and thumbs on the sides of the scalp
3. Palms and thumbs on the sides of the scalp- Perform this exercise for 5 minutes at each of the three positions (for a total of 15 minutes) every evening at bedtime.
- Begin the exercise 8 weeks prior to surgery (when possible) and continue the exercise up to the day before your procedure.
Removing the Donor Strip
Tumescent Anesthesia
A major advancement in the removal of the donor strip is the use of tumescent anesthesia. Tumesce simply means to expand by injecting fluid into the tissues. In this technique, very dilute concentrations of anesthetic fluid are injected into the fat layer of the donor region of the scalp. This serves a number of purposes, the first is to decrease bleeding from the pressure of the fluid on small blood vessels (capillaries), the second is to firm the skin so that the incision can be more easily controlled and third, to increase the distance between the follicles and the deeper tissues of the scalp. This helps the surgeon keep the incision superficial so that the larger nerves and blood vessels in the scalp are not injured and so that the fascia is not cut. The fascia is a layer of fibrous tissue that lies just below the fat layer that gives support to the scalp. If this layer is cut, the risk of having a stretched scar significantly increases.
Undermining
Undermining, the technique of separating the upper layers of the scalp from the lower portions in the area around the wound edges can be useful if there is excessive tension on the wound edges during the closure. This is occasionally needed when the scalp is tight, when a patient has had multiple prior hair transplant procedures or when the donor strip was too wide. Undermining, however, can increase the risk of bleeding, nerve injury and trauma to the scalp and may result in poor healing. Although undermining is a very useful tool in some situations, it is generally best to avoid the need for undermining entirely by carefully planning the donor incision.
Donor Closure
Staples
The advantage of using staples is that, of all the donor closures, staples conserve the most hair. There are two main reasons for this. The first is that stainless steel staples are inert. This means that, unlike sutures, the body tissues do not react to them and therefore staples cause minimal inflammation (which has the potential to damage hair follicles). The second advantage of staples is that they are interrupted, in contrast to sutures which are used in a long running loop stitch. A running stitch had a tendency to strangle hair follicles, particularly if there is any swelling after the surgery. The use of interrupted staples avoids this potential damage to grafts.
The advantage of sutures had been that the surgeon had the most control in approximating (closing together) the wound edges. For a long time, we felt that the better control of the wound edges offered by sutures outweighed its disadvantages. However, with new stapling techniques and modifying the time that the staples are left in the scalp, excellent wound edge approximation is achieved and the main advantage of sutures has largely been eliminated.
Sutures are generally more comfortable post-operatively than staples and are more convenient for patients because they do not need to be removed. However, because staples offer superior preservation of donor hair, this is our closure of choice for most procedures. For those patients who will benefit from sutures, or for those who simply prefer them, we still offer this type of closure.
 Appearance of typical stapled closure six weeks post-op.
Appearance of typical stapled closure six weeks post-op. Note that there is little trace of donor area scar even with the hair cut relatively short.
Note that there is little trace of donor area scar even with the hair cut relatively short.Absorbable Sutures
Monocryl is a synthetic absorbable suture with very low tissue reactivity. It is absorbed by hydrolysis (dissolved by the water in tissues rather than by an inflammatory response) so that there is minimal damage to follicles. After introducing the use of Monocryl sutures to hair transplantation in 2001, we continued to use this suture material for a number of years (see Dr. Bernstein’s publication “New Suture for Hair Transplantation“). The advantage of this closure is patient comfort, the convenience of not having to be removed and the complete control of the wound edges (which is felt to result in superior healing). However, in spite of these benefits, we now prefer to use staples in the majority of our cases due to the ability of stapled closures to best preserve the patient’s donor hair supply (see Staples above).
Trichophytic “Tricho” Closure
In a trichophytic closure, the surgeon makes the initial incision parallel to the hair follicles and then trims away 1 to 3-mm of tissue of either the upper or lower wound edge (or both), so that the top of the hair follicles at that wound edge are removed. During the “tricho” closure, the trimmed wound edge is pulled towards the opposite edge so that the bottom parts of the cut hairs are pointing slightly towards the incision (rather than parallel to each other). The goal is that these hairs will eventually grow through the incision and thus decrease the visibility of the scar.
In the upper ledge trichophytic closure, the hair from the upper wound edge points down and grows into the scar. In the lower ledge trichophytic closure, the hair in the lower wound edge grows through the overlapping upper edge.
Trichophytic closures generally require the wound edges to be sutured. The benefit of a trichophytic closure is less when staples are used. The advantage of staples is that this closure enables the maximum conservation of donor hair. The doctor will decide which would be optimal in your case.








